Downloads
Download the Pre-Travel Consultation Guidelines
Please click here to download the Pre-Travel Consultation Guidelines.
Download the Pre-Travel Patient Checklist
Please click here to download the Pre-Travel Patient Checklist.
Acronyms
| AIH | Australian Immunisation Handbook |
| AIR | Australian Immunisation Register |
| AMS | Acute Mountain Sickness |
| APTHS | Asia Pacific Travel Health Society |
| BCG | Bacille Calmette-Guerin |
| CDC | Centers for Disease Control |
| COVID-19 | Corona Virus Disease - 2019 |
| DEET | N, N-diethyl-meta-toluamide |
| DVT | Deep vein thrombosis |
| ECG | Electrocardiogram |
| FiO2 | Fraction of inspired oxygen |
| HBV | Hepatitis B virus |
| HIV | Human Immunodeficiency Virus |
| ICVP | International Certificate of Vaccination or Prophylaxis |
| HACE | High altitude cerebral oedema |
| HAPE | High Altitude pulmonary oedema |
| ID | Intradermal |
| IM | Intramuscular |
| IGRA | Interferon Gamma Release Assay |
| ISTM | International Society of Travel Medicine |
| JE | Japanese Encephalitis |
| JEG | Japanese Encephalitis Guidelines |
| LMIC | Low and Middle Income Countries |
| MMR | Measles, mumps and rubella |
| MMRV | Measles, mumps, rubella and varicella |
| MSM | Men who have sex with men |
| NaTHNaC | National Travel Health Network and Centre |
| NIR | National Immunisation Register (NZ) |
| NZ | New Zealand |
| OLE | Oil or lemon eucalyptus |
| ORS | Oral rehydration solution |
| OTC | Over the counter |
| PAHO | Pan American Health Organization |
| PDC | Professional Development Certificate |
| PEP | Post Exposure Prophylaxis |
| SARS-Co-V2 | Severe Acute Respiratory Infection Coronavirus 2 |
| TB | Tuberculosis |
| TD | Traveller’s Diarrhoea |
| THP | Travel Health Professional |
| TST | Tuberculin skin testing |
| UK | United Kingdom |
| VFR | Visiting friends and relatives |
| WHO | World Health Organization |
| THNANZ | Travel Health Nurses of Australian and New Zealand |
| YF | Yellow Fever |
Purpose of Guideline
The purpose of this guideline is to outline the pre-travel consultation and provide a suggested plan for undertaking these consultations as well as considerations for means of gathering information that may aid in this process.
It also provides considerations for those who may wish to establish a travel medicine clinic.
Introduction
- The pre-travel consultation is essential for identifying travel related risks for the individual (both specific and general), educating the traveller about specific travel hazards and providing prevention strategies such as vaccinations, medications and other recommendations that may be useful for the traveller.
- The traveller should ideally consult the practitioner 4-61-2 weeks prior to travel to ensure sufficient time to optimise any health conditions, provide any vaccinations required and ensure the traveller has received sufficient education and/or is guided towards relevant health information. There will be occasions where the intending traveller attends too late to develop a scheme for advised vaccine recommendations. See Appendix 1 ‘The Last-Minute Traveller’ for tips on how to manage this situation.
- Optimally, the traveller should inform the practice when booking the consultation, that it is a travel related consultation to allow sufficient time to be allocated. The patient could be asked to bring relevant information and arrive earlier to complete a travel checklist. Information required includes vaccination history, medical history (if not a regular patient of the practice), list of all medications (prescribed, over the counter, herbal etc).
- However, as patients rarely volunteer this information when booking appointments, a patient new to the practice may arrive without relevant information or having completed a checklist. The consultation may need to be delayed allowing time for the traveller to complete the checklist and/or the traveller may need to return for additional consultations (depending on patient factors, proposed travel itinerary etc).
- There is an opportunity with online booking apps to include travel consultation in the options when making the appointment. This could include a prompt to inform the patient to arrive 20 minutes earlier than appointment to complete the checklist and/or provide an online checklist to pre-fill prior to the appointment. Relevant information the patient is advised to take to the consultation could also be included in the prompts when making the booking.
- The consultation between the intending traveller and the travel health professional (THP) is an essential way of individualising health and safety information according to perceived risks in the intended travel. Such information is dependent upon intended destination(s), and length, type, and time of travel.
- The risk to travellers includes various communicable diseases as well as injuries, accidents or other travelled related conditions and therefore a personalised risk assessment for each person is required.
- If couples, family members or friends attend the same booking, determine if discussions surrounding medical history can be held in their presence (note privacy). Longer consultation times will be required for additional persons attending the consultation.
- The practitioner can provide comprehensive education to the traveller and/or provide them with information sheets and links to further information, according to their individual needs and requirements. It is essential that all information provided (verbal and written) is recorded in the patient file.
- The practitioner should only provide travel advice when they feel competent and confident to do so. Medico-legal issues may arise if appropriate advice is not provided and/or if the practitioner fails to recommend appropriate vaccinations or malaria chemoprophylaxis in high risk travel areas. Where practitioners have knowledge gaps, referral to a specialist including specialist travel practitioners is essential. See Establishing a Travel Clinic for more information regarding this.
- Increasingly it is becoming more common for patients to request virtual consults which is advantageous particularly for those in regional and remote areas where no specialist travel services exist. It would be advantageous to the practitioner if the patient checklist is completed and submitted, and a review of all previous vaccinations is checked prior to the consult (from AIR/NIR and/or patient’s yellow book). The practitioner should ensure all items discussed during a face-to-face consultation are included in the virtual consult. Where the patient may require vaccines and/or specific medications and they are unable to attend the practice where the virtual consult was held, a letter should be provided to the patient to take to their preferred practitioner with these recommendations.
- Patient - Download pre-travel patient checklist form
- - to fill in prior to consultation (where possible)
- Trip details
- Destinations
- Departure date and length of trip
- Transport type – aircraft, sea, train, road
- Accommodation – all that is planned e.g. hotels, visiting friends and relatives (VFR), hostels, camping; rural/urban; ocean/mountains/desert/tropics
- Activities planned – skiing, bushwalking/hiking, water sports (kayak, swimming, diving), climbing/altitude, cycling, motorcycling, other
- Previous travel history (and any problems/experiences)
- Travel insurance
- Medical history
- Allergies (including anaphylaxis) – to medications, egg, other
- Previous vaccinations including any adverse events
- Medications – name, dose, frequency (include all prescribed even if irregular, contraception, over the counter, vitamins, herbal, other)
- List of possible medical conditions (by system - respiratory, cardiac, renal, liver, haematological, endocrine, neurological, GI, autoimmune, pregnancy, previous surgery); past and present
- Last dental visit
- Trip details
- - to fill in prior to consultation (where possible)
- Practitioner
Details of the proposed trip along with personal factors will determine the discussions the consultation will require. The practitioner should use the patient checklist as a guide to the consultation.
Duration and destination are important - spending a 2 to 3 week holiday in a western country (Europe, United Kingdom, North America) will have different risks than a longer holiday or if backpacking through Asia, Africa, Central or South America.
Age of the person will be important for certain risks e.g. younger travellers are more likely to be involved in higher risk activities such as motorcycle riding whereas older patients may have co-morbidities that may make them more susceptible to infections or complications from disease or medications.- Trip details (as above)
- Destinations
- Departure date and length of trip
- Transport type – aircraft, sea, train, road
- Accommodation – all planned e.g. hotels, VFR, hostels, camping; rural/urban; ocean/mountains/desert/tropics
- Activities planned – skiing, bushwalking/.hiking, water sports (kayak, swimming, diving), climbing/altitude, cycling, motorcycling, other
- Previous travel history (and any problems/experiences)
- Medical history
It is necessary to go through patient’s checklist carefully (or ask patient if checklist is not completed). Compare with patient record if regular clinic patient
- ask about any allergies including type of reaction
- ask about all previous vaccinations and adverse events (check patient file, Australian Immunisation Register/National Immunisation Register (NZ))
- record all medications including prescribed, OTC, vitamins, herbal, other. Include irregular or periodic medications e.g. Prolia
- clarify status of previous and current medical conditions (stable, routine monitoring etc); past surgery (splenectomy, transplantation); pregnancy or planned pregnancy
- Trip details (as above)
High risk travellers
Travellers who have a higher risk of infections or ill health whilst travelling include:
- Patients with chronic medical conditions e.g. diabetes, renal disease, autoimmune diseases, obesity, malignancies etc
- Patients on specific medications e.g. corticosteroids, immunomodulating drugs, warfarin
- Pregnant women
- Children
- Travellers visiting friends and relatives especially in low and middle income (LMIC) countries
- Expatriates
- Backpackers
The practitioner should explain thoroughly if travel is very high risk e.g. if a pregnant woman will spend time in a highly malarious area, the practitioner may recommend she reconsider her travel.
Once information has been gathered from the patient, practitioner should focus on the following:
- Are any vaccinations required?
- Education of risks and recommendations for prevention of infections, accidents and altitude sickness in this person and their planned destination(s).
- Does the traveller require any malaria chemoprophylaxis or other medications to reduce risks or self-treat during travel?
Practitioners should be aware of the risk of vaccine preventable diseases including those with lesser risk but high consequence if infected. See graphic below showing those infections that are high risk but those with low risk but high consequence3.
Figure 1. Vaccine preventable disease travel health risks: Estimated incidence per month in lower income countries…
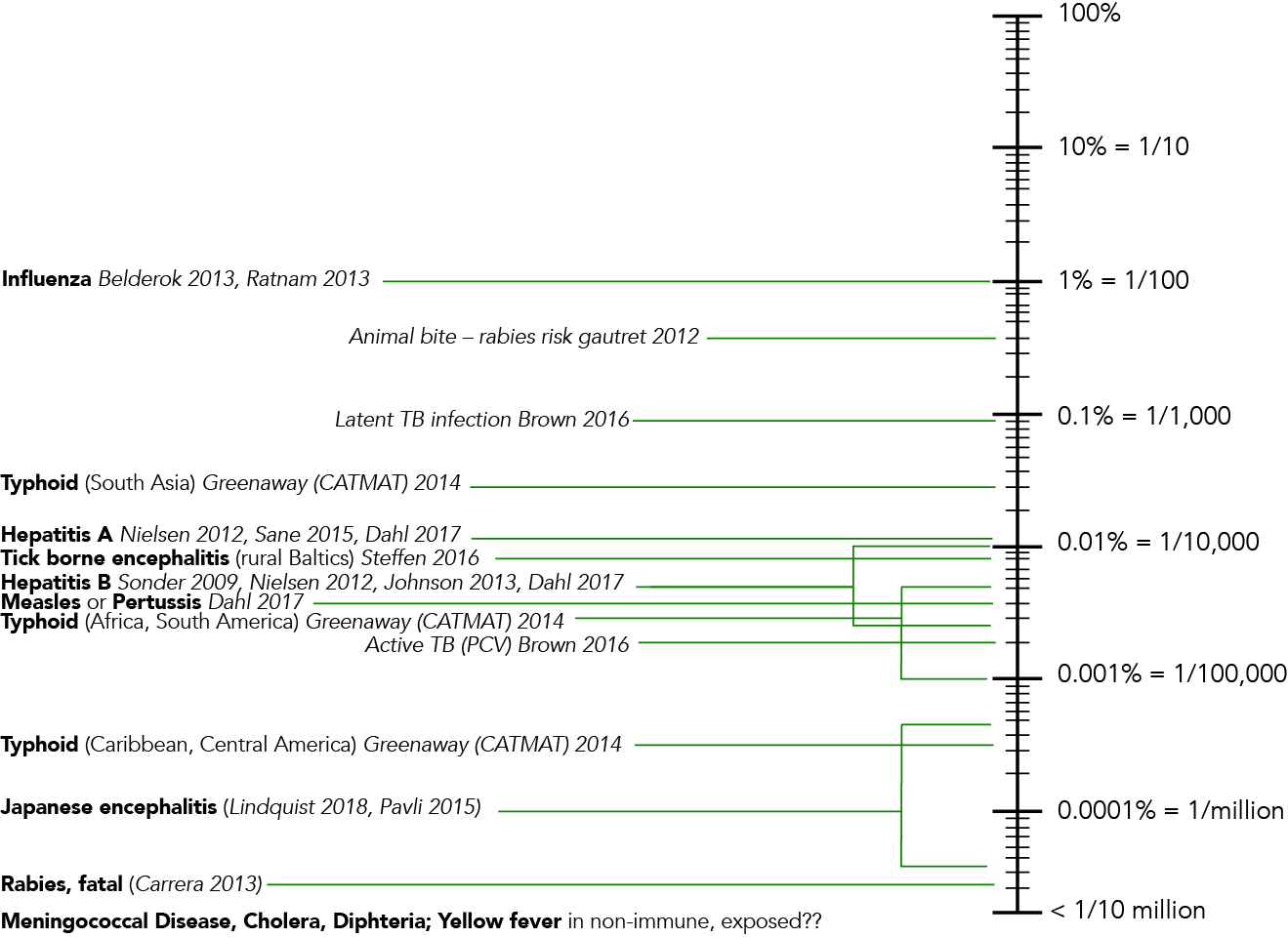
J Travel Med, Volume 25, Issue 1, 2018, tay046, https://doi.org/10.1093/jtm/tay046
Vaccinations
- Discuss routine vaccines that are recommended for the individual that is specific to their age and medical conditions but not specifically travel related. These will include being up to date with all childhood vaccinations, including: tetanus, diphtheria, pertussis, polio, measles, meningococcal, HBV and may include varicella, influenza and pneumococcal vaccines for those with risk factors or above a certain age. Travellers may be at increased risk of exposure during travel e.g. diphtheria, measles, polio hence travellers should be clear why these vaccinations should be kept up to date.
- Discuss recommended vaccines based on age of traveller, itinerary, activities and risk of exposure to disease e.g. typhoid, hepatitis A, hepatitis B, Japanese encephalitis, rabies, dengue fever, meningococcal ACWY +/- B, influenza, tuberculosis, yellow fever, tick borne encephalitis.
- Discuss required vaccines for entry into certain countries or required by International Health Regulations e.g. SARS-Co-V2, Yellow Fever, Meningococcal ACWY, polio (as appropriate for proposed trip).
Type of Vaccine Routine – up to date with vaccines specific to age and medical conditions (not specifically travel related): Tetanus
Diphtheria
Pertussis
Polio
Measles
Meningococcal
HBV
Varicella
Influenza
Pneumococcal
Recommended based on
- - age
- - itinerary
- - activities
- - risk of exposure
Typhoid
Hepatitis A
Hepatitis B
Japanese Encephalitis
Rabies
Meningogococcal ACWY, B
Influenza
Tuberculosis
Yellow fever
Dengue fever*
Tick borne encephalitis*
Required - for entry into certain countries or required by International Health Regulations Yellow Fever
SARS Co-V2
Meningococcal ACWY
Polio
* Recommended for some travellers. Currently needs to be imported into both countries. Seek expert advice.
For more information on vaccinations for international travel see here and here.
For a list of vaccinations by destination see recommendations from: Australia, CDC and UK.
Practitioner needs to:
- consider whether there is time to provide recommended vaccines prior to departure and/or whether an accelerated schedule is required. Young children may require routine vaccines at the minimum age rather than recommended age particularly if visiting countries with a high risk of vaccine preventable diseases such as measles4. See minimum age for vaccinating children in Australia (table), New Zealand (handbook). See Appendix 2 for a list of vaccines that can be given as an accelerated schedule
- ensure traveller is aware of cost of vaccines. Some travellers may consider vaccinations recommended are too expensive however it is important to counsel and discuss the ramifications of not being vaccinated and becoming infected and unwell whilst travelling (including possible long-term outcomes such as ongoing hepatitis, inability to work etc)
- checklist for contraindications to vaccinations (Australia5, NZ6) prior to prescription
- Perform live vaccine check list
- History of egg allergy generally not a contraindication (see Australia7, NZ8)
- Pregnancy/breastfeeding
- Have other live vaccines been administered within 4 weeks? Ensure live vaccines are administered on the same day (otherwise 28 days is required between doses (excluding oral live vaccines (typhoid, polio and rotavirus) which can be administered at any time interval). One Brazilian study in children under 2 years, suggested yellow fever and MMR should be given at least 30 days apart to improve seroconversion rates hence where sufficient time may allow administration 30 or more days apart, seroconversion rates may be higher9. Where time may not permit this, an alternative would be to check serology for measles, mumps and rubella and if negative and both vaccines are required, inform the patient seroconversion may be suboptimal. See Appendix 3 Live vaccines for a list of live vaccines.
- Has the patient received blood or blood products (immunoglobulin) within 12 months? (Australia10, New Zealand11)
- Immunocompromised e.g. is patient on immunosuppressive drugs, having chemotherapy or radiotherapy? (Australia12, New Zealand13).
- If no medical contraindications, document in patient file
- Explain and preferably provide a handout of possible side effects of all vaccines
- If verbal consent provided, document in patient records; if written consent, include signed consent in patient’s notes (patient also needs to be provide explicit verbal consent even if written consent is provided at a previous consultation)
- All vaccines provided should be recorded in the patient’s electronic record and where possible, the national immunisation register (if no automatic software link). Where the patient is required to have written proof of vaccination such as yellow fever, the yellow book also needs to be completed.
- Specific vaccines
- Yellow fever vaccination must be given by an accredited centre and documented on the International Certificate of Vaccination or Prophylaxis (ICVP) document (yellow book)
- For travellers who are required to receive the polio vaccine or meningococcal (ACWY) for travel, documentation is also required on a new page in the International Certificate of Vaccination or Prophylaxis (ICVP)
Education about Risks
Food and water
(see Food and Water guideline for more detailed information - coming soon)
- Provide education on the risk of infections from contaminated food, water and ice. Bacteria (including E. coli, Salmonella spp, Campylobacter jejuni, Shigella spp), viruses (Hepatitis A, E, norovirus, rotavirus) and parasites (Giardia lamblia, E, histolytica) are all common causes of gastrointestinal infection in travellers with patients often experiencing vomiting, diarrhoea, abdominal pain and other symptoms.
- Prevention strategies can be discussed and should include information about good personal hygiene, drink boiled/treated/bottled water, eat hot and well-cooked food/avoid pre-cooked food, raw meat & seafood, avoid salads unless vegetables cleaned in boiled/treated water. Travellers are advised to eat at locations which are busy, have a good turn-over of food, and have locals eating at them. Provide information sheets for travellers to read such as here and here.
- Vaccination for Salmonella Typhi and Hepatitis A is advised if the traveller is visiting areas of endemicity (diseases are often endemic in low and middle income countries and in areas of poor sanitation).
- Travellers with liver disease or those immunosuppressed are strongly encouraged (regardless of travel destination) to have Hepatitis A vaccine to avoid severe disease.
- Travellers should be up to date with polio vaccine which remains endemic in some countries. See here for a list of countries with polio outbreaks. Some countries may require polio vaccination and an international certificate (ICVP) as a condition of entry. See here for information about polio by destination Australia, New Zealand.
- Treatment of travellers’ diarrhoea (TD) depends on the severity, impact on activities and duration of symptoms. Appropriate treatment always includes ensuring adequate fluid intake preferably with oral rehydration solution.
- Prophylactic antibiotics are not routinely recommended due to the high risk of adverse effects including promotion of drug resistant bacteria14.
- An anti-motility agent should not be routinely recommended but may be useful where travellers can’t delay their travel and diarrhoea may be problematic e.g. long trips (road or air).
- Anti-motility medications should not be used in children or if the traveller has fever or bloody stools.
- Antibiotics for treatment are not recommended unless there is blood in the stools, the traveller has severe diarrhoea (incapacitated and unable to participate in planned activities) and where traveller is immunocompromised. One dose of azithromycin is recommended with additional dose or change of antibiotics only if there is no improvement. See Food and Water guideline (Coming soon) and here for more details.
- Provision of a TD treatment kit is recommended for most travellers (see below); the contents will vary depending on the individual’s risk factors (age, medical conditions, style of travel and activities planned), season and destination of travel (which would determine the most prevalent intestinal pathogens) and access to adequate local medical facilities.
TD TREATMENT KIT Basic kit contents include - oral rehydration sachets
- an antimotility agent (e.g. loperamide) if not contraindicated and
- an antibiotic known to be effective in all regions but only recommended under specific circumstances e.g. azithromycin. See Food and Water guideline (Coming soon) for more information
A more advanced kit might also contain - an anti-emetic such as metoclopramide or ondansetron
- an anti-spasmodic such as hyoscine butylbromide (buscopan) and
- an anti-parasitic agent such as metronidazole.
- A detailed description including written instructions of how and when to use the various contents and when to seek medical advice is essential.
Arthropod Borne Diseases
(See additional links for guidelines and more comprehensive information for arthropod-borne diseases guidelines, malaria guidelines and Japanese encephalitis guidelines.)
- The most important message to convey to travellers is ‘no bite = no disease’.
- Viruses, bacteria and parasites can be transmitted to humans through the bite of arthropods, many of which can cause severe disease including fatalities.
- Knowledge of planned activities and specific vector-borne disease risks at all destinations are necessary to provide the best advice on prevention.
Arthropods most likely to affect travellers, and the diseases that they transmit, include the following:
| Arthropods causing potentially serious infections in Travellers | |
| Mosquitoes | |
| day-time biting - Aedes spp | Dengue fever Chikungunya Yellow Fever Zika |
| night time biting - Anopheles spp |
Malaria Filaria |
| night time biting - Culex spp | Japanese Encephalitis Filaria West Nile fever |
| Ticks | Lyme disease (Borrelia burgdorferi) Tick-borne encephalitis African tick bite fever (Rickettisa africae) |
| Mites | Scrub typhus (Orientia tsutsugamushi) |
| Fleas | Murine typhus (Rickettsia typhi) Plague (Yersinia pestis) Relapsing Fever (Borrelia recurrentis) |
| Lice | Epidemic Typhus (Rickettsia prowazekii) |
| Flies | Sandflies (Leishmaniasis) Tse tse (African trypanosomiasis) Black (Onchocerciasis) Myiasis
|
| Triatomine bugs | American trypanosomiasis |
Adapted from WHO Vector-borne Diseases (2020).15 For additional information see here.
Bite Prevention
It is essential to educate travellers to take precautions such as
- avoid bites (of all arthropods) wherever possible
- use of effective repellents (including DEET, picaridin or OLE) and other insecticides (mosquito coils, electrical vaporising mats)
- long sleeved tops and trousers to reduce amount of bare skin; permethrin treated clothes, sleeping sheets and equipment
- sleep under impregnated mosquito nets or in rooms with flyscreens
- avoid activities from dusk until dawn (to prevent night biting mosquitoes)
- check for ticks, mites after activities that increase risk of exposure; shower soon after activity completed
- Other ‘things’ that do not work such as Vitamin B, noise buzzers
Malaria
(See Malaria guidelines for more information.)
- Night-time biting Anopheles spp mosquitoes are vectors for Malaria
- Access to detailed malaria information and/or maps is vital for the practitioner to check whether the traveller will be visiting a malaria area. The information should clearly indicate areas of risk, peak season, urban vs rural, drug-resistance, and predominant parasite species. For specific country information see CDC (more risk averse than other recommendations), Travel Health Pro (UK), Fit for Travel (UK) and Public Health England.
- Education of the traveller is paramount
- location of the risk areas in itinerary
- prevention through avoiding mosquito bites
- malaria symptoms to be aware of both during and post-travel (fever, chills, headache, myalgia)
- possible prescription of chemoprophylaxis (see below)
- information on diagnostic and treatment options (see malaria guidelines) including possible standby treatment
- avoid travel if pregnant or asplenia since high risk of severe malaria
- Chemoprophylaxis options need to be explained fully, including costs, side effect profiles and dosing schedules. Chemoprophylaxis should be considered for all travellers visiting malarious areas. Risk is higher in many African countries particularly West Africa. In SE Asia, the risk is often less, particularly in the dry season.
- A conversation should be had with each traveller going to a risk area to outline the risk of malaria and need to use all preventive measures as described above as well as a discussion of chemoprophylaxis.
- More detailed discussion should be had with those who are at risk of more severe malaria such as children, pregnant women and those with asplenia/hyposplenism. In some cases, such as pregnant women, you may recommend they do not go on the trip due to the risk, or that they change their itinerary to avoid visiting at risk areas. Those who initially come from a malarious area, often have had malaria multiple times in their lives but their immunity to severe malaria is lost once they have lived in a non-malarious area for longer than approximately 18 months. They are often not aware that they are at risk of severe disease if returning to their birthplace.
- For those travelling for extended periods, taking chemoprophylaxis long term may not be an attractive option. If they are going to live in a risk area long term they may start by taking malaria tablets until they are settled, have all prevention measures in place and sought out potential medical facilities for management if they do develop malaria.
- Backpackers may not wish to take it long term either. Provision of stand by prophylaxis if they develop malaria may be an option, particularly if they may be somewhere remote without immediate access to medical care.
- Please refer to malaria guideline for further information.
- See here for
- Australia and New Zealand travel medicine malaria guideline (Coming soon)
- malaria information by country – CDC, Travel Health Pro (UK)
- recommendations for prevention and prophylaxis
- CDC Malaria information
Japanese Encephalitis
(See JE guideline for more information.)
- Dusk and Night-time biting Culex spp mosquitoes are vectors for JE.
- JE is a vaccine preventable disease that is a significant public health problem in many parts of Asia and the Western Pacific. The risk of infection in travellers is largely dependent on season and duration of travel, style of accommodation, activities planned, and whether it involves rural/repeat/expatriate or VFR travel.
- JE is classified as a low risk, high consequence disease with those becoming symptomatic having a high risk of severe illness and death. See Japanese Encephalitis Guidelines (JEG) for additional information.
- Prevention of infection includes:
- avoiding dusk to dawn Culex mosquito species bites by using effective insect repellents, contact insecticide, mosquito nets/coils, staying in screened accommodation
- vaccination is recommended for travellers spending one month or more in endemic areas in Asia and Papua New Guinea during the wet season or those travelling less than a month but may have ongoing travel (frequent, shorter trips), are travelling during wet season, experience considerable outdoor activity or sleeping in rooms without screens or nets. See JEG for more information on vaccines
- For more information see here.
Dengue, Chikungunya and Zika Infections
(See ABD guidelines for more information – coming soon)
- The vectors for Dengue fever, Chikungunya and Zika are Aedes aegypti (predominantly) and Ae. albopictus mosquitoes which are daytime-feeding and inhabit densely populated areas. Peak biting times are dawn and dusk however they can bite at any time during the day (particularly if it is overcast). Both species have a preference for mammalian blood, however Aedes aegypti are more likely to feed on humans.
- The global distribution of both species combined is wide and increasing due to climate change, with populations becoming established in more temperate climates and at higher altitudes. Dengue fever and chikungunya are considered a risk in more than 10016,17 countries and to date, 89 countries and territories have reported evidence of Zika virus infection.18
- Common symptoms for all three viruses are fever, headache, muscle pain, joint pain and rash. Severe disease can occur in dengue (but is more common in secondary infections) whereas Zika and Chikungunya are more likely to produce acute and chronic symptomatology.
- Pregnant women should avoid infection at any stage during their pregnancy as Zika may cause microcephaly and other neurological effects in new-borns. Those planning a pregnancy should avoid travelling to Zika risk areas prior to pregnancy. It is recommended to wait for 3 months if travel has been made to a Zika risk area prior to pregnancy. If a woman is pregnant and her partner travels to a risk area, safe sex should be practiced for the remainder of the pregnancy.
- Due to their predilection for urban habitats and mammalian blood, the mosquitoes capable of transmitting dengue fever, chikungunya and Zika virus are a substantial risk for most travellers to at-risk areas – even cruise day-trippers spending a day in port. As a result, insect bite prevention measures must be explained fully.
- Dengue vaccination is currently not recommended for all travellers, though may be advised for those who have had the disease previously and who plan to visit an endemic area for a long period e.g. expatriate. Newer vaccines are available in some countries and as the disease becomes more of a public health threat, recommendations for vaccination for some travellers may change.
- No vaccination is available for Chikungunya or Zika viruses.
- For risk maps see here: dengue, chikungunya and Zika.
- For more information see guidelines and also dengue, chikungunya and Zika
Yellow Fever
- Yellow fever is a mosquito-borne viral infection that can be severe and cause death.
- The vector for Yellow Fever in urban areas is predominantly the Aedes aegypti which are daytime-feeding and inhabit densely populated areas. These mosquitoes are also responsible for transmission of dengue fever, chikungunya and Zika virus. In rural areas, additional Aedes species as well as Haemagogus and Sabethes species are also vectors. Most disease occurs in rural areas (jungle and savannah) rather than urban areas where the disease is periodic or sporadic19. Travellers working in or partaking in activities in rural areas need to be aware of the risks of disease.
- Travellers 9 months and older travelling to a yellow fever transmission country (tropical and subtropical areas of Africa and Central and South America) may be recommended or required to be vaccinated against the disease. See vaccine recommendations from WHO, for Australia20 and New Zealand.21
- Maps of transmission and vaccination recommendations can be found here: Africa, Central and South America.
- Many countries require a valid International Certificate of Vaccination or Prophylaxis (ICVP) against yellow fever (or letter of exemption) if the traveller arrives from a country of known risk of transmission.
- Travel health practitioners will need to check entry requirements for countries the traveller intends to visit (including transit for 12 or more hours) prior to departure. See CDC, WHO and PAHO for more details. For Australian information see here and here and New Zealand here.
- Practitioners require training and certification to provide the vaccine otherwise they must refer to a specialised centre (Australia, New Zealand). Online training is available: Australia, New Zealand.
- All travellers will need to be educated about avoiding mosquito bites (even when vaccinated), wearing appropriate clothing and using personal insect repellents. See 'Bite Prevention' above malaria section.
- For more information on Yellow Fever vaccination see Australia, New Zealand and CDC.
Ticks and mites
- Travellers who engage in bushwalking, camping and other outdoor activities are at risk of being bitten by mites and ticks in endemic areas.
- Serious infections include scrub typhus (mite-borne) found in Asia/Pacific, tick borne infection of Lyme disease (Europe, North Asia and North America) and Tick-borne encephalitis (Europe, North Asia). A vaccine for tickborne encephalitis is available.
- Travellers are advised to be fluent about the use of insect repellents, permethrin treated clothes and equipment during activities. They need to be encouraged to check for mites and ticks at the end of the activity and shower soon after where possible.
Flies
- Flies can transmit diseases including sleeping sickness (Trypanosomiasis), river blindness (Onchocerciasis) and Leishmaniasis. Travellers visiting game parks in some parts of Africa are at risk of tsetse fly bites (Trypanosomiasis) and are therefore encouraged to wear lightly coloured long sleeved shirts, long pants and hats. Blue and black colours are to be avoided since the flies appear to be attracted to these colours and may bite through clothing of these colours.
- Myiasis can occur in South, Central America and Africa. Ironing clothes will prevent infection by killing eggs of the fly.
Rabies
(See Rabies guideline for more information.)
- Most Australian and New Zealand travellers lack an awareness of the potential risk of rabies or other lyssavirus infection. Infection is caused by exposure to saliva or neural tissue from an infected animal e.g. usually a dog, but can also be a bat, cat, monkey or any other mammal and is almost always fatal once symptoms appear. Humans can be exposed through a bite or scratch that breaks the skin or direct contact of the virus with the person’s mucosa (nose, eye, mouth).22
- A risk assessment for vaccination is recommended for expatriates or travellers visiting rabies endemic areas where:
- there is limited access to immediate medical care
- when contact with animals is anticipated.
- Areas where rabid dogs are common include Africa, Asia, Central and South America. Bats anywhere are a potential source of lyssavirus.
- Travellers are advised to avoid contact with all animals when travelling even if the animal appears well.
- If bitten, scratched or mucosa is in direct contact with a potentially infected animal or bat, it is essential to wash the area well with soap and water. Flush with copious amounts of water for at least 15 minutes.23 Application of povidone-iodine or alcohol may be useful to also reduce bacterial infection. Do not suture or cover wound. Seek immediate medical care including post exposure prophylaxis (even if pre-exposure vaccine has been provided). See table below.
- Many endemic countries do not offer either post exposure prophylaxis (PEP) or immunoglobulin and therefore pre departure vaccination is highly recommended for those at risk. Various pre-exposure schedules exist including:
- the recommended 3 dose schedule (day 0, 7, 21-28 by IM or ID injection)24
- an accelerated schedule is also possible –
- day 0, 3, 7 (3 doses IM) or
- days 0, 7 (2 injections each day ID) i.e. 4 doses. Intradermal route should only be given by suitably qualified and experienced providers.
- For travellers receiving an accelerated schedule, a booster 12 months after the first dose will improve antibody response.
- For travellers older than 50 years, seroconversion rates are higher with the 3-day schedule hence this is recommended over the 2-day ID schedule. If the 2-day schedule is given, a fifth booster dose at 12 months provides long term immunity comparable to 3 dose schedule.25
Table: Categories of contact and recommended post-exposure prophylaxis (PEP)26
| Categories of contact with suspect rabid animal | Post-exposure prophylaxis measures |
| Category I - touching or feeding animals, animal licks on intact skin (no exposure) | Washing of exposed skin surfaces, no PEP |
| Category II - nibbling of uncovered skin, minor scratches or abrasions without bleeding (exposure) | Wound washing and immediate vaccination |
| Category III - single or multiple transdermal bites or scratches, contamination of mucous membrane or broken skin with saliva from animal licks, exposures due to direct contact with bats (severe exposure) | Wound washing, immediate vaccination and administration of rabies immunoglobulin/monoclonal antibodies |
Category II and III exposures require PEP.
- For more information on rabies see:
- Australia
- Australia and New Zealand Travel guidelines (Coming Soon)
- WHO including map of endemicity
Blood and Body Fluid Borne Infections
- HIV, Hepatitis B and C can be transmitted via contact with contaminated blood, blood products and other bodily fluids including semen (HIV, Hepatitis B and rarely Hepatitis C).
- Education should be provided about high-risk behaviours which include: unprotected sex, sharing drug injection equipment, poor infection control practices (poor processing of medical/dental equipment including for body piercing and tattooing, use of multi-dose vials for injections is common in some LMIC) and unscreened blood for transfusions.
- Hepatitis B vaccination should be offered to all those travelling to endemic areas as well those at higher risk of HIV (visit sex workers, casual sexual encounters, men who have sex with men (MSM) or people with multiple, casual partners).27 Hepatitis B vaccine can be given as a combination with Hepatitis A. See here for more information on combination vaccines: Australia/New Zealand and Appendix 2 for accelerated schedule.
- For more information on hepatitis B see Australia/New Zealand.
- International travellers should also be advised that some countries have entry and exit requirements for individuals with AIDS infection. See here for more information.
- Travellers at risk of HIV may also consider pre-exposure prophylaxis, an effective preventative HIV infection option.
COVID-19
- Infection from SARS-CoV-228 virus remains a problem with frequent surges in infections in most countries. All travellers should be up to date with recommended vaccinations and those at higher risk of severe disease should be aware of what they can do whilst travelling to reduce their risk.
- See COVID-19 Guidelines28 for more information.
Meningococcal meningitis
- Vaccination is recommended for travellers visiting areas where epidemics of serogroups A, C, W or Y meningococcal disease occur (particularly sub-Saharan Africa).29 See map here.
- Vaccination for both MenB and MenACWY vaccines is also recommended for travellers (particularly adolescent and young adults), who will stay in hostels or dormitory accommodation during travel.
- Proof of vaccination is required for entry when visiting the Hajj into Saudi Arabia. See here and here for more details.
- For more information see WHO, vaccine recommendations for Australia here and here; New Zealand.
Influenza
- Those at higher risk for severe illness from influenza should be up to date with their vaccination prior to travel.
- Vaccination for all travellers should be considered if travelling to a destination with an influenza epidemic, if travelling on a cruise, in a large tourist group (particularly one that includes older persons) or if participating in mass gatherings.
Destination specific topics to consider
High Incidence Tuberculosis countries
- Children under 5 years are at highest risk of severe disease from tuberculosis when visiting or living in a country of high incidence (≥40/100,000). The longer the exposure, the greater the risk of infection. Vaccination with BCG is most effective at preventing severe TB (miliary and tuberculous meningitis) in this age group.
- Australia and New Zealand differ a little in their recommendations for vaccination of children under 5 years.
- In Australia a risk assessment is recommended for children under 5 years who:
- have parents from high incident countries: BCG is not routinely recommended due to low TB incidence in Australia but parents should consider vaccination if there is a risk of exposure (e.g. from themselves if recently in high incident country, relatives visiting them in Australia or if travel to place of parent’s origin if planned (see no. 2 below)
- those who will travel and/or live in high incidence countries. The risk assessment should consider the age of the child, TB incidence at destination(s), proximity of contact with others (VFR increases risk), length of time exposed (the longer the stay and/or multiple trips under 5 years increases the risk of infection).30 Health practitioners should discuss with families as early as possible e.g. during a pregnancy so if the risk of exposure is high, there will be sufficient time to have the child vaccinated before potential exposure from visiting family members or travel.
- The need for a tuberculin skin test prior to vaccination should also be determined by an individual risk assessment.31 See here for more details. Seek expert advice from State or Territory TB/Chest clinics or paediatric infectious diseases.
- New Zealand currently recommends vaccination in children under 5 years who:
- have one or both parents or household members or carers who within the last five years lived for a period of six months or longer in countries with a TB rate of ≥40/100,000 or
- During their first five years will be living for 3 months orf longer in a country with a TB rate ≥40/100,00032
- Children offered BCG at birth or within the first 6 months of life do not require tuberculin skin testing (TST) or interferon gamma release assay (IGRA) (unless family member is a known TB patient where clinical screening may be advised).
- Vaccinating older children and adults is less beneficial and not routinely recommended.
- Vaccination should ideally be given at least 3 months before departure to a high risk destination. Other live vaccinations can be given at the same time or after 4 weeks (MMR, yellow fever, varicella). TST/IGRA should be performed prior to vaccination if over 6 months of age to rule out previous infection.
- See WHO, Australian Immunisation Handbook and New Zealand Immunisation Handbook for more information.
Schistosomiasis
- Schistosomiasis is a parasitic disease caused by trematode worms. There are two major clinical forms – urogenital and intestinal caused by various species. The majority of schistosomiasis infections occur in sub-Saharan Africa (Schistosoma mansoni and S. haematobium), but other areas of transmission include Middle East, Caribbean and more recently in Corsica, Europe as well as China and SE Asia (intestinal form due to S. japonicum, S. mekongi).
- Travellers returning to see friends and relatives as well as ‘adventure’ travellers are most at risk of infection. Infections occur when larval forms of the parasite penetrate the skin during contact with fresh water (swimming, bathing, wading and fishing in rivers, lakes or smaller bodies of water).
- Prevention is through avoiding this contact in known areas of infection. Water for bathing should be boiled and cooled prior to use or left standing for a day (provided no snails are present). Wear boots or waders if crossing an at-risk watercourse. Swimming in chlorinated pools or the ocean is safe.
- For travellers who have been exposed, serology can be obtained 3 months after exposure and if positive can be treated (this does not apply to those who are from schistosomiasis endemic regions or those who have previously lived in an endemic region).
Travel to areas of High Altitude
- The practitioner needs to provide advice to travellers who are planning to spend time at or above 2500m so history of travel plans and activities are essential.
- Altitude illness can occur in any traveller ascending to 2500 m or higher unless they are acclimatised. Both children and adults are susceptible with no screening tests to predict the risk.
- As one ascends, the fraction of inspired oxygen (FiO2) decreases (normal FiO2 is 21%) which can lead to hypoxic stress:
- At 2,500m = FiO2 is 15%
- 3,500m = 14%
- 4,500m = 12%
- If a person has experienced acute mountain sickness (AMS) (or the more severe outcomes of rapid ascent), they are likely to suffer it again under the same conditions.
- Most people will tolerate an ascent to 2,500 metres with minimal effects, however above this AMS symptoms may become apparent
- Three factors influence the risk of developing illness:
- Elevation at destination
- Rate of ascent
- Amount of exertion
- There are three syndromes of altitude sickness:
- Acute Mountain Sickness (AMS). This is the most common and is similar to a ‘bad hangover’ - headache, loss of appetite, nausea, fatigue, dizziness, disturbed sleep and occasionally vomiting. Periodic breathing is common during sleep at high altitudes.
- High Altitude Pulmonary Oedema (HAPE) develops after 2 or 3 days of altitudes above 2500m. Initially they are breathless on exertion and will also have symptoms of AMS. Cough is often present and may be associated with white or pink frothy sputum. The person becomes weak and then develops breathlessness at rest. Symptoms are similar to chest infection however without treatment (descent, oxygen) the condition can be fatal.
- High Altitude Cerebral Oedema (HACE) is a severe form of AMS but is fortunately rare. The person becomes increasingly confused, drowsy, unsteady and ataxic. Death can occur within hours, so descent is essential.
- Prevention
- The best preventive strategy for altitude illness is gradual ascent to allow acclimatisation. Ideally travellers should take 2 or more days to ascend to an initial 3000metres, with subsequent increases in sleeping elevation of no more than 500metres each day
- Avoid going from low elevation to more than 2800m in one day
- Once at 3000m, sleep no higher than 500m each night
- Take a rest day with each 1,000m climb
- Climb high, sleep low
- Consider using acetazolamide to speed acclimatisation if abrupt ascent is unavoidable
- Avoid alcohol (at least for initial 48 hours)
- Avoid smoking and sedatives
- Recognise symptoms early
- Do not ascend further if experiencing any symptoms of altitude illness. If mild symptoms, wait until acclimatised before ascending further. If more severe symptoms, descent is imperative
- Acetazolamide
- Start the day before ascent and continue to maximum altitude. If staying at the same altitude, acetazolamide can be stopped after 2 or 3 days as traveller will be acclimatised.
- Adults: 125mg 12 hourly.
- Children: 5mg/kg/day to max 250mg/day in 2 divided doses.
- Acetazolamide contains a sulfa moiety but carries an extremely low risk of inciting an allergic reaction in persons with sulfonamide allergy. As a result, persons with known allergy to sulfonamide medications can consider a supervised trial of acetazolamide before the trip, particularly if planning travel to a location remote from medical resources.33
- Side effects include paraesthesia of face, hands, feet, frequent urination (adequate fluid intake important at altitude), bitter or metallic taste, nausea, vomiting, diarrhoea.
- Dexamethasone can be used as an alternative prophylactic to acetazolamide for adult travellers where the latter may be contra-indicated. Although not as good as acetazolamide, there is indeed a benefit in using dexamethasone in AMS prevention. Whilst the drug is not advised for AMS prevention in children, the recommended adult doses are 2 mg every 6 h or 4 mg every 12 h. It is not generally advised for use for more than 10 days, but if it is then it needs to be tapered off over a week and not stopped suddenly.34
- Treatment of Altitude Illness
- Descent is the definitive treatment for severe AMS, HAPE and HACE.
For additional information on altitude illness including treatment see here and here.
Establishing a Travel Clinic
Introduction
As practitioners, time management can be problematic however it is essential for those providing travel advice that sufficient time is allotted to ensure the patient has an adequate risk assessment and all advice including vaccinations, medications are provided to the traveller.
Suggestions for different levels of service are presented below:
Level 1: General Practitioner and Nurse Routine Consults
Level 2: General Practitioner Specialisation in Travel Health
Level 3: Travel Medicine Specialist Nurse
Level 4: Travel Medicine Specialist Doctor
- For Level 1 and 2: ‘The Consultation in General Practice’ – questions to be asked include:
- How to maximise consultation agenda in the time available?
- What to discuss and how to plan this?
- Roles of the doctor and nurse in consultation need to be defined
- A practice nurse is essential and needs to be upskilled
- Time is the major factor- What is the minimum time required to perform a travel consultation? Our opinion is that a minimum of 20 minutes is required to provide a travel medicine consultation. If 20 minutes is not possible then patients need to be referred to specialist services (in person or virtual).
- For Level 3 and 4: ‘The Specialised Consultation in Travel Health’
- Those with an interest in global and travel health will need to be pro-active in the management of travellers in the future and look much further than vaccinations and anti-malarial advice.
- The prescriptive tools for the future are clear and laid out for those who wish to grow into a new and exciting re-boot of post COVID-19 travel medicine: a rejuvenated, prescriptive and ongoing post-graduate education, current geographical and historical sources and best possible global political resources including an atlas.
Offering travel medicine services - Preparation
The first steps in the process of establishing a travel medicine service must include determining which services will be provided i.e., a one-stop shop for vaccines, medications such as anti-malarials, first aid and treatment kits and products including insect repellents, mosquito nets, water purifiers and other travel accessories. Are the vaccines and prescription medications to be ordered and stocked by the clinic or obtained from a pharmacy? In addition, it will be necessary to establish whether the practice has available:
- Clinicians – doctors or nurse practitioners - as well as practice nurses who have an interest in travel medicine, have undertaken training in the field (or who are willing to do so) and agree to maintain currency through ongoing study or attending educational sessions (conferences, webinars, self-directed learning).
- Session time and consultation rooms to manage a stream of new travellers.
- Consultation times which include those that may be more suitable for those studying or working during ‘office hours’ i.e., after-hours and weekends.
- Spare capacity of lockable storage of medications, products and kits, as well as the vaccines necessary for the prevention, vaccine fridge, management and treatment of a full range of travel health risks (if clinic is to provide all of the above to travellers).
- Access to travel health resources i.e., a travel medicine database supplying up-to-date and accurate information on epidemiology or disease risk/outbreaks, maps of disease endemicity, seasonal variations, transmission, malaria maps and vaccination requirements.
- Travel health information in hard copy to provide to travellers i.e., insect bite prevention, information on common travel-related illnesses, how to manage travellers’ diarrhoea.
- Suitably trained administrative staff who can manage scheduling of appointments, information gathering and complex billing.
- Awareness of laws regarding labelling of medications as applies to the state of residence.
Ongoing education for travel health professionals
- In order to be able to prescribe the yellow fever vaccine it is necessary to follow the federal government regulations as well as complete training module on providing the vaccine. (See Yellow fever Accreditation in section below under Administration.)
- Online training is available: Australia, New Zealand.
- Formal training in travel medicine is provided in the Graduate Certificate of Travel Medicine at James Cook University, Queensland and a Postgraduate Certificate in Travel Medicine at the University of Otago in New Zealand.
- Developing expertise in travel medicine can also be achieved through self-directed study of online resources for health professionals providing care to international travellers, including:
- CDC Yellow Book: Health Information for International Travel
- UK National Travel Health Network and Centre (NaTHNaC)
- the Manual of Travel Medicine 4th Ed (2019)
- Australian Immunisation Handbook
- New Zealand Immunisation Handbook and
- the World Health Organisation (WHO).
- Australasian College of Tropical Medicine
- The International Society of Travel Medicine (ISTM) conducts a virtual Travel Medicine Review and Update Course, as well as the Certificate in Travel Health™ exam – also virtual.
- The Professional Development Certificate (PDC) in Travel Medicine from the Royal College of Physicians and Surgeons of Glasgow, UK, has been designed to enhance the knowledge and skills of doctors, nurses and pharmacists working within Travel Medicine. The course’s four core modules take in pre-Travel Risk Assessment & Management, Travel-related Infections, Malaria and Mosquito-borne Diseases, and Immunology and Immunisations.
- As it is of the utmost importance to be up-to-date in the field, membership of international and regional societies, which were formed to promote and advocate for travel health, is highly recommended. Institutions such as the ISTM and the Asia Pacific Travel Health Society (APTHS) provide networking opportunities, as well as hosting webinars and conferences on relevant subject matter. Benefits of ISTM membership also include a special members-only online community offering access to special travel medicine alerts, links to important resources, members only discussion groups, publications, educational products and biennial conferences. Australasian College of Tropical Medicine also has an annual Travel and Tropical medicine conference.
- Dependent on the practitioner’s level of knowledge, ensure to identify travel consultations you are prepared to do and those which you may refer to a specialist service.
Offering travel medicine services - Administration
- Provide induction to receptionists so they are aware of the need to ask callers if appointment is travel-related and provide a set process to complete booking. (See next point.)
- Prepare a template or use checklist for travel health bookings which includes destinations, length of trip, transport type (aircraft, ship etc) etc.
- Include in template the appointment length allowed for different types of consultations i.e., longer for families with children, complicated itineraries, complex medical history.
- Need to request traveller brings relevant medical documentation (including government accepted documentation such as Medicare number, a list of all medications) and vaccination history (may include previous vaccination book(s)).
- Pre-consult patient checklist (see under consultation) to be completed by traveller prior to consultation. Ideally, to save time, email executable PDF in advance or request traveller arrives at practice early to complete paperwork.
- Accreditation is required to be a yellow fever vaccinator and also a vaccination centre. Applications for approval as a Yellow Fever Vaccination Centre are made to the relevant health authority. Details of the process in gaining accreditation: Australia - National Guidelines for Yellow Fever Vaccination Centres and Providers; for New Zealand see here.
- Criteria used to indicate compliance with the guidelines may include:
- The practice has at least one practitioner accredited to administer the vaccine.
- The practice’s cold chain management strategies are in line with National guidelines. Evidence of this could be through practice accreditation or another mechanism approved by the state or territory health authority.
- The practice has the ability to treat adverse effects, including anaphylaxis.
- The practice records evidence of valid informed consent.
- The practice has access to up-to-date travel advisory and travel health information for practitioners to provide patients with advice on mosquito protection and safe travel practices in tropical countries.
- The practice has the ability to retain an accurate record of yellow fever vaccination history.
- Practice nurses must be proficient in vaccine management - cold chain, ordering and patient recalls, as well as having access to the online immunisation handbooks of Australia and New Zealand for information on vaccine indications, schedules and contraindications etc. They may also be involved in stock management of kits, treatment and anti-malarial medications, insect repellent and any other travel health accessories.
- Immunisation updates offered by local public health units are a good starting point for most vaccine information, however those used in travel health are not a priority. Local/regional support for nurses working in travel health is available for members of the Travel Health Nurses of Australia and New Zealand (THNANZ), affiliated with the ACTM.
Offering travel medicine services - Prior to each session
- Ensure adequate stock on hand prior to commencing each session: vaccines, medications (prophylaxis and treatment), first aid or treatment kits, yellow fever vaccination booklets, exemption letters/medication authority templates, products (i.e., insect repellent, travellers’ diarrhoea treatment or first aid kits) and hard copies of patient information.
- Check of anaphylaxis protocols and treatments in place.
- Ensure checks of all relevant updates of significant or notable disease outbreaks or relevant news items.
- Gather relevant paperwork: checklists, patient information, yellow vaccination booklets & stamp, medication authority forms.
- Check vaccine, medication, accessory stocks.
- Take repellents, products to consulting room.
- Read through current travel health news/alerts e.g. EPIWATCH and Health Map.
- Open travel health software or free national services e.g.
Appendix 1 The Last Minute Traveller
It is not uncommon for a patient to see her/his usual GP and at the end of the consultation say ‘by the way we are going to X in 2 weeks. Is there anything special I need to do?’
This poses a dilemma for the GP since it takes time to take a travel history and provide the necessary information to the patient. It is not ideal to have a short consultation however if the patient cannot return for a full consult, cannot have a telehealth/virtual consult (and/or there is insufficient time to do so), then the minimum requirements include:
- Destinations/Length of time/activities – this will help tailor the consultation
- Vaccinations – consider accelerated schedule if insufficient time e.g. HBV, rabies, measles (if infant not yet vaccinated and 6 – 12 months of age)
- Provide education regarding
- risks for their type of travel and need for them to check whether destinations will have malaria, require certain vaccines e.g. YF, MenACWY etc.
- take precautions not to be bitten by insects and animals, sleep in screened rooms/under nets, have safe sex/take condoms, don’t take unnecessary risks (wear a helmet etc).
- Take double usual medication. Separate into 2 packs and put in different areas of luggage in case of baggage loss
- Provide info sheets particularly on malaria if going to an endemic area, prevention and management of TD, reducing risk of bites etc
- Strong recommendation for health insurance.
Our recommendation however, is that the practitioner should encourage for a full travel consultation either in person or virtually rather than providing a quick and insufficient consultation.
Appendix 2 Accelerated Schedule
Suggested accelerated vaccination schedule if required for traveller
| Vaccine | Suggested accelerated schedule |
| Hepatitis B | Day 0, 7, 21 and 12 months35 |
| Hepatitis A & B | Day 0, 7, 21 and 12 months36,37 |
| Measles | Can be given from 6 months of age but will require additional 2 doses from age of 12 months38,39 |
| MenACWY/MenB | Vaccination at 6 weeks of age is possible but additional doses may be required. See local guidelines for individual vaccine recommendations: Australia,40,41,42,43 New Zealand44. Seek expert advice if necessary |
| Rabies | Day 0, 3, 7 IM or Day 0, 7 - 2 injections each time ID Recommended to have another dose 12 months after first dose45 |
Appendix 3 Live vaccines
Live vaccines
| Parenteral | Japanese Encephalitis (Imojev) MMR – measles, mumps, rubella MMRV – measles, mumps, rubella, varicella Varicella Yellow fever Zoster BCG |
| Oral | Rotavirus (oral) Typhoid Polio (no longer offered in Australia or New Zealand) |
References
1 Shaw, M. (2006). Running a travel clinic. Travel medicine and infectious disease, 4(3-4), 109–126. https://doi.org/10.1016/j.tmaid.2005.06.006
2 Leder, K. and Weller, P. F. (2021). Travel Advice. In T. W. Post, D. J. Sexton and E. L. Baron, (Eds.), UptoDate, available from https://www.uptodate.com/contents/travel-advice?search=travelers%20diarrhea&source=search_result&selectedTitle=3~102&usage_type=default&display_rank=3#H5
3 Steffen, R. (2018). Travel vaccine preventable diseases—updated logarithmic scale with monthly incidence rates, Journal of Travel Medicine, 25(1) https://doi.org/10.1093/jtm/tay046
4 Australian Technical Advisory Group on Immunisation. (2021, September 27). Table. Minimum acceptable age for the 1st dose of scheduled vaccines in infants. In Australian Immunisation Handbook https://immunisationhandbook.health.gov.au/resources/tables/table-minimum-acceptable-age-for-the-1st-dose-of-scheduled-vaccines-in-infants accessed December 17, 2022.
5 Australian Technical Advisory Group on Immunisation. (2023, January 25). Table. Pre-vaccination Screening Checklist. In Australian Immunisation Handbook https://immunisationhandbook.health.gov.au/resources/tables/table-pre-vaccination-screening-checklist accessed April 7, 2023.
6 Ministry of Health. (2023, April 11). Table 2.2: Pre-vaccination screening and actions to take. In Immunisation Handbook 2020. Wellington: Ministry of Health. https://www.health.govt.nz/our-work/immunisation-handbook-2020/2-processes-safe-immunisation#table2-2 accessed on May 5, 2023.
7 Australian Technical Advisory Group on Immunisation. (2019, April 23). Vaccinating people with a known egg allergy. In Australian Immunisation Handbook https://immunisationhandbook.health.gov.au/contents/vaccination-for-special-risk-groups/vaccination-for-people-who-have-had-an-adverse-event-following-immunisation#vaccinating-people-with-a-known-egg-allergy accessed December 17, 2022
8 Ministry of Health. (2023, April 11). Egg allergy. In Immunisation Handbook 2020. Wellington: Ministry of Health. https://www.health.govt.nz/our-work/immunisation-handbook-2020/11-influenza#10-6-3 accessed on May 5, 2023.
9 Nascimento Silva J.R., Camacho, L. A., Siqueira, M. M., et al. Mutual interference on the immune response to yellow fever vaccine and a combined vaccine against measles, mumps and rubella. Vaccine, 2011, 29(3). https://doi.org/10.1016/j.vaccine.2011.05.019
10 Australian Technical Advisory Group on Immunisation. (2022, December 7). Vaccination for people who have recently received normal human immunoglobulin and other blood products. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/contents/vaccination-for-special-risk-groups/vaccination-for-people-who-have-recently-received-normal-human-immunoglobulin-and-other-blood-products accessed December 17, 2022.
11 Ministry of Health. (2022, August 30). Table A6.1: Suggested intervals between immunoglobulin and blood product administration or blood transfusion and MMR or varicella vaccination. In Immunisation Handbook 2020. Wellington: Ministry of Health. https://www.health.govt.nz/our-work/immunisation-handbook-2020/appendix-6-passive-immunisation#tablea6-1 accessed on September 1, 2022.
12 Australian Technical Advisory Group on Immunisation. (2023, January 30). People on immunosuppressive therapy. In Australian Immunisation Handbook https://immunisationhandbook.health.gov.au/contents/vaccination-for-special-risk-groups/vaccination-for-people-who-are-immunocompromised#people-on-immunosuppressive-therapy accessed April 7, 2023.
13 Ministry of Health. (2023, April 11). Immunocompromised individuals. In Immunisation Handbook 2020. Wellington: Ministry of Health. https://www.health.govt.nz/our-work/immunisation-handbook-2020/4-immunisation-special-groups#4-3 accessed on May 5, 2023.
14 Riddle, M.S., Connor, B. A., Beeching, N.J., DuPont, H.L., Hamer, D.H., Kozarsky, P., Libman, M., Steffen, R., Taylor, D., Tribble, D.R., Vila, J., Zanger, P and Ericsson, C.D. (2017). Guidelines for the prevention and treatment of travelers' diarrhea: a graded expert panel report. Journal of Travel Medicine, 24 (suppl_1):S57-S74. doi: 10.1093/jtm/tax026
15 World Health Organisation. (2020, March 2). Vector Borne Diseases https://www.who.int/news-room/fact-sheets/detail/vector-borne-diseases accessed on November 1, 2022.
16 World Health Organisation. (2023). Dengue and severe dengue, https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue accessed March 3, 2023
17 World Health Organisation. (2022, December 8). Chikungunya https://www.who.int/news-room/fact-sheets/detail/chikungunya accessed December 1, 2022.
18 World Health Organisation. (n.d.). Zika Virus Disease, https://www.who.int/health-topics/zika-virus-disease#tab=tab_1 accessed August 3, 2023.
19 Gershman, M. D. and Staples, J. E. (2021), Yellow Fever. In G. W. Brunette and J. B. Nemhauser (Eds.), CDC Yellow Book 2020, Oxford University Press. https://wwwnc.cdc.gov/travel/yellowbook/2020/travel-related-infectious-diseases/yellow-fever accessed April 6, 2023.
20 Australian Technical Advisory Group on Immunisation (ATAGI). (2022, May 19). Yellow Fever. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/contents/vaccine-preventable-diseases/yellow-fever#travellers accessed on March 1, 2023.
21 Te Whatu Ora Health New Zealand. (2023). Yellow Fever, https://www.tewhatuora.govt.nz/for-the-health-sector/health-sector-guidance/diseases-and-conditions/yellow-fever accessed on March 1, 2023
22 Australian Technical Advisory Group on Immunisation. (2018, June 6). Rabies and other Lyssavirues. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/contents/vaccine-preventable-diseases/rabies-and-other-lyssaviruses accessed April 6, 2023.
23 World Health Organisation. (2023). Rabies. https://www.who.int/news-room/fact-sheets/detail/rabies accessed April 6, 2023.
24 Australian Technical Advisory Group on Immunisation. (2018, June 6). Rabies and other Lyssavirues. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/contents/vaccine-preventable-diseases/rabies-and-other-lyssaviruses accessed April 6, 2023.
25 Furuya-Kanamori L, Ramsey L, Manson M, Gilbert B, Lau CL. Intradermal rabies pre-exposure vaccination schedules in older travellers: comparison of immunogenicity post-primary course and post-booster. J Travel Med. 2020 Nov 9;27(7) https://doi.org/10.1093/jtm/taaa006
26 World Health Organisation. (2023). Rabies. https://www.who.int/news-room/fact-sheets/detail/rabies accessed April 6, 2023.
27 Australian Technical Advisory Group on Immunisation. (2022, December 7). Hepatitis B in Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/contents/vaccine-preventable-diseases/hepatitis-b Accessed on May 5, 2023.
28 Travel Medicine Clinical Guidelines Australia and New Zealand. (n.d.). Australian COVID-19 International Travel Guidelines https://www.travelmedicineguidelinesanz.org/covid-19-information.php accessed on Nov 30, 2022.
29 Australian Technical Advisory Group on Immunisation. (2022, December 7). Meningococcal Disease. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/contents/vaccination-for-special-risk-groups/vaccination-for-international-travellers#meningococcal-disease accessed December 17, 2022.
30 Australian Technical Advisory Group on Immunisation. (2022, August 5). Tuberculosis – Travellers. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/contents/vaccine-preventable-diseases/tuberculosis#travellers accessed April 6, 2023.
31 Australian Technical Advisory Group on Immunisation. (2022, August 5). Tuberculosis – Tuberculin skin testing before vaccination. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/contents/vaccine-preventable-diseases/tuberculosis#tuberculin-skin-testing-before-vaccination accessed April 15, 2023.
32 Ministry of Health. (2022, December 8). Tuberculosis – Recommended Immunisation Schedule, in Immunisation Handbook 2020. https://www.health.govt.nz/our-work/immunisation-handbook-2020/21-tuberculosis#20-5 accessed April 6, 2023.
33 Luks, A. M., Swenson, E. R. Medication and dosage considerations in the prophylaxis and treatment of high-altitude illness. Chest. 2008;133(3):744e55
34 Luks, A. M., Auerbach, P. S., Freer, L., Grissom, C. K., Keyes, L. E., McIntosh, S. E., Rodway, G. W., Schoene, R. B., Zafren, K., & Hackett, P. H. (2019). Wilderness Medical Society Clinical Practice Guidelines for the Prevention and Treatment of Acute Altitude Illness: 2019 Update. Wilderness & environmental medicine, 30(4S), S3–S18. https://doi.org/10.1016/j.wem.2019.04.006
35 Australian Technical Advisory Group on Immunisation. (2018, June 5). Table. Accelerated hepatitis B vaccination schedules for people with imminent risk of exposure. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/resources/tables/table-accelerated-hepatitis-b-vaccination-schedules-for-people-with-imminent-risk-of-exposure accessed on May 5, 2023.
36 Australian Technical Advisory Group on Immunisation. (2018, June 5). Table. Accelerated hepatitis B vaccination schedules for people with imminent risk of exposure. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/resources/tables/table-accelerated-hepatitis-b-vaccination-schedules-for-people-with-imminent-risk-of-exposure accessed on May 5, 2023.
37 Ministry of Health. (2021, August 17). Table 8.2: Hepatitis A- containing vaccines: by age, dose and schedule. In Immunisation Handbook 2020. Wellington: Ministry of Health. https://www.health.govt.nz/our-work/immunisation-handbook-2020/8-hepatitis#table7-2 accessed on May 5, 2023.
38 Australian Technical Advisory Group on Immunisation. (2022, May 9). Measles – Travellers. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/contents/vaccine-preventable-diseases/measles#travellers accessed on May 5, 2023.
39 Ministry of Health. (2022, December 15). Measles. 12.5. Rapid Immunisation Schedule. In Immunisation Handbook 2020. Wellington: Ministry of Health. https://www.health.govt.nz/our-work/immunisation-handbook-2020/12-measles#11-5 accessed on May 5, 2023.
40 Australian Technical Advisory Group on Immunisation. (2021, September 27). Table. Minimum acceptable age for the 1st dose of scheduled vaccines in infants. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/resources/tables/table-minimum-acceptable-age-for-the-1st-dose-of-scheduled-vaccines-in-infants accessed on May 5, 2023.
41 Australian Technical Advisory Group on Immunisation. (2022, December 7). Table. Recommendations for immunisation of infants and children aged < 2 years using meningococcal ACWY vaccines, by age and vaccine brand. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/resources/tables/table-recommendations-for-immunisation-of-infants-and-children-aged accessed on May 5, 2023.
42 Australian Technical Advisory Group on Immunisation. (2022, December 7). Table. Recommendations for immunisation of infants and children aged < 2 years using meningococcal B vaccine. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/resources/tables/table-recommendations-for-immunisation-of-infants-and-children-aged-0 accessed on May 5, 2023.
43 Australian Technical Advisory Group on Immunisation. (2022, December 7). People who travel to areas where meningococcal disease is more common, or who travel to mass gatherings, are strongly recommended to receive MenACWY vaccines. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/recommendations/people-who-travel-to-areas-where-meningococcal-disease-is-more-common-or-who-travel-to-mass-gatherings-are-strongly-recommended-to-receive-menacwy-vaccines accessed on May 5, 2023.
44 Ministry of Health. (2023, April 11). 13. Meningococcal Disease 13.4 Vaccines. In Immunisation Handbook 2020. Wellington: Ministry of Health. https://www.health.govt.nz/our-work/immunisation-handbook-2020/13-meningococcal-disease#12-4 accessed on May 5, 2023.
45 Australian Technical Advisory Group on Immunisation. (2021, September 21). People who work with bats, laboratory workers who work with live lyssaviruses and some people who travel to rabies-enzootic areas are recommended to receive rabies vaccine as pre-exposure prophylaxis. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/recommendations/people-who-work-with-bats-laboratory-workers-who-work-with-live-lyssaviruses-and-some-people-who-travel-to-rabies-enzootic-areas-are-recommended-to-receive-rabies-vaccine-as-pre-exposure-prophylaxis accessed on May 5, 2023
All references, links and bibliography
General Travel Information and Planning for Travel
Leder, K. and Weller, P. F. (2021). Travel Advice. In T. W. Post, D. J. Sexton and E. L. Baron, (Eds.), UptoDate, available from https://www.uptodate.com/contents/travel-advice?search=travelers%20diarrhea&source=search_result&selectedTitle=3~102&usage_type=default&display_rank=3#H5
Shaw, M. (2006). Running a travel clinic. Travel medicine and infectious disease, 4(3-4), 109–126. https://doi.org/10.1016/j.tmaid.2005.06.006
Torresi, J., McGuinness, S., Leder, K., O’Brien, D., Ruff, T., Starr, M. and Gibney, K. Manual of Travel Medicine (4th Ed). (2019). Springer. Available from https://doi.org/10.1007/978-981-13-7252-0
National Travel Health Network and Centre. (n.d.). Travel Health Pro, UK Health Security Agency. https://travelhealthpro.org.uk accessed on Sep 1, 2022.
National Travel Health Network and Centre. (2022, July 21). Travel Health Pro EBook. UK Health Security Agency. https://travelhealthpro.org.uk/ebook.php#book5/page1 accessed April 7, 2023.
National Travel Health Network and Centre. (n.d.). Protecting the health of the British Traveller. UK Health Security Agency. https://nathnac.net accessed on Sep 1, 2022.
Centers for Disease Control and Prevention. (2020). CDC Yellow Book 2020: Health Information for International Travel. Oxford University Press https://wwwnc.cdc.gov/travel/page/yellowbook-home accessed April 6, 2023.
Centers for Disease Control and Prevention. (n.d.). Traveler’s Health. U.S. Department of Health and Human Services https://wwwnc.cdc.gov/travel/ accessed on November 30, 2022.
Tools to assist travel practitioner / Checklist
Department of Foreign Affairs and Trade. (n.d.) Smartraveller, Australian Government. https://www.smartraveller.gov.au accessed April 6, 2023.
Ministry of Foreign Affairs and Trade. (n.d.) Safetravel, New Zealand. https://www.safetravel.govt.nz accessed April 6, 2023.
Massachusetts General Hospital. (n.d.). GlobalTravelEpiNet, Pre-Travel Providers’ Rapid Evaluation Portal (Pre-Travel PREP), Boston, Massuchusetts. https://gten.travel/prep/prep accessed on April 6, 2022.
Centers for Disease Control and Prevention. (n.d.). Traveler’s Health, Destinations. U.S. Department of Health and Human Services. https://wwwnc.cdc.gov/travel/destinations/list accessed on November 30, 2022.
Centers for Disease Control and Prevention. (2022, November 3). Traveler’s Health, Clinician Resources. U.S. Department of Health and Human Services. https://wwwnc.cdc.gov/travel/page/clinician-information-center accessed on April 6, 2023.
Centers for Disease Control and Prevention. (n.d.). Traveler’s Health, Disease Directory. U.S. Department of Health and Human Services. https://wwwnc.cdc.gov/travel/diseases accessed on April 6, 2023.
National Travel Health Network and Centre. (n.d.). Country Information, UK Health Security Agency. https://travelhealthpro.org.uk/countries accessed on Sep 1, 2022.
Vaccinations
General Information
Australian Technical Advisory Group on Immunisation (ATAGI). (2022). Australian Immunisation Handbook, Australian Government Department of Health and Aged Care, Canberra. https://immunisationhandbook.health.gov.au
Ministry of Health. (2020). Immunisation Handbook 2020. Wellington: Ministry of Health. https://www.health.govt.nz/our-work/immunisation-handbook-2020
Steffen, R. (2018). Travel vaccine preventable diseases—updated logarithmic scale with monthly incidence rates, Journal of Travel Medicine, 25(1) https://doi.org/10.1093/jtm/tay046
Freedman, D. O. and Leder, K. (2023). Immunizations for Travel. In T. W. Post, P. F. Weller, and E. L. Baron, (Eds.), UptoDate, available from https://www.uptodate.com/contents/immunizations-for-travel?search=live%20vaccines&source=search_result&selectedTitle=10~150&usage_type=default&display_rank=10 accessed on April 7, 2023.
World Health Organisation. (2019). Vaccine-preventable diseases and vaccines. In International Travel and Health https://cdn.who.int/media/docs/default-source/travel-and-health/9789241580472-eng-chapter-6.pdf?sfvrsn=8c1a400c_14 accessed Nov 1, 2022.
Specific vaccine requirements for IHR or specific destinations
Australian Technical Advisory Group on Immunisation. (2022, December 7). Vaccines required by the International Health Regulations or for entry into specific countries. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/contents/vaccination-for-special-risk-groups/vaccination-for-international-travellers#vaccines-required-by-the-international-health-regulations-or-for-entry-into-specific-countries accessed December 17, 2022.
Vaccines for international travellers
Australian Technical Advisory Group on Immunisation. (2022, December 7). Vaccination for International Travellers. In Australian Immunisation Handbook https://immunisationhandbook.health.gov.au/contents/vaccination-for-special-risk-groups/vaccination-for-international-travellers accessed December 17, 2022.
Department of Health. (n.d.) Vaccination for International Travellers. Australian Government. https://immunisationhandbook.health.gov.au/sites/default/files/2021-07/Publication-Vaccination-for-international-travellers.pdf accessed December 17, 2022.
Ministry of Health. (2020). Immunisation of special groups – Travel. In Immunisation Handbook 2020. Wellington: Ministry of Health. https://www.health.govt.nz/our-work/immunisation-handbook-2020/4-immunisation-special-groups#4-9 accessed on September 1, 2022.
Minimum age for 1st vaccine dose e.g. if travelling prior to 1st recommended vaccine
Australian Technical Advisory Group on Immunisation. (2021, September 27). Table. Minimum acceptable age for the 1st dose of scheduled vaccines in infants. In Australian Immunisation Handbook https://immunisationhandbook.health.gov.au/resources/tables/table-minimum-acceptable-age-for-the-1st-dose-of-scheduled-vaccines-in-infants accessed December 17, 2022.
Vaccines for special groups and contraindications
Pre-vaccination screening checklist
Australian Technical Advisory Group on Immunisation. (2023, January 25). Table. Pre-vaccination Screening Checklist. In Australian Immunisation Handbook https://immunisationhandbook.health.gov.au/resources/tables/table-pre-vaccination-screening-checklist accessed April 7, 2023.
Assessing those with previous adverse reactions and special groups
Australian Technical Advisory Group on Immunisation. (2019, April 23). Vaccination for people who have had an adverse event following immunisation. In Australian Immunisation Handbook https://immunisationhandbook.health.gov.au/contents/vaccination-for-special-risk-groups/vaccination-for-people-who-have-had-an-adverse-event-following-immunisation accessed December 17, 2022.
Ministry of Health. (2020). Table 2.2: Pre-vaccination screening and actions to take. In Immunisation Handbook 2020. Wellington: Ministry of Health. https://www.health.govt.nz/our-work/immunisation-handbook-2020/2-processes-safe-immunisation#table2-2 accessed on September 1, 2022.
Ministry of Health. (2020). Immunisation of Special Groups. In Immunisation Handbook 2020. Wellington: Ministry of Health. https://www.health.govt.nz/our-work/immunisation-handbook-2020/4-immunisation-special-groups accessed on September 1, 2022.
Egg allergy
Australian Technical Advisory Group on Immunisation. (2019, April 23). Vaccinating people with a known egg allergy. In Australian Immunisation Handbook https://immunisationhandbook.health.gov.au/contents/vaccination-for-special-risk-groups/vaccination-for-people-who-have-had-an-adverse-event-following-immunisation#vaccinating-people-with-a-known-egg-allergy accessed December 17, 2022.
Ministry of Health. (2020). Egg allergy. In Immunisation Handbook 2020. Wellington: Ministry of Health. https://www.health.govt.nz/our-work/immunisation-handbook-2020/11-influenza#10-6-3 accessed on September 1, 2022.
Recent immunoglobulin and blood products
Australian Technical Advisory Group on Immunisation. (2022, December 7). Vaccination for people who have recently received normal human immunoglobulin and other blood products. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/contents/vaccination-for-special-risk-groups/vaccination-for-people-who-have-recently-received-normal-human-immunoglobulin-and-other-blood-products accessed December 17, 2022.
Ministry of Health. (2020). Table A6.1: Suggested intervals between immunoglobulin and blood product administration or blood transfusion and MMR or varicella vaccination. In Immunisation Handbook 2020. Wellington: Ministry of Health. https://www.health.govt.nz/our-work/immunisation-handbook-2020/appendix-6-passive-immunisation#tablea6-1 accessed on September 1, 2022.
Immunocompromised individuals
Australian Technical Advisory Group on Immunisation. (2023, January 30). People on immunosuppressive therapy. In Australian Immunisation Handbook https://immunisationhandbook.health.gov.au/contents/vaccination-for-special-risk-groups/vaccination-for-people-who-are-immunocompromised#people-on-immunosuppressive-therapy accessed April 7, 2023.
Ministry of Health. (2020). Immunocompromised individuals. In Immunisation Handbook 2020. Wellington: Ministry of Health. https://www.health.govt.nz/our-work/immunisation-handbook-2020/4-immunisation-special-groups#4-3 accessed on September 1, 2022.
Vaccines recommended for destinations
Australia
Department of Foreign Affairs and Trade. (n.d.), Smartraveller Destinations. Australian Government. https://www.smartraveller.gov.au/destinations accessed on April 5, 2023.
Other
Centers for Disease Control and Prevention. (n.d.). Traveler’s Health, Destinations. U.S. Department of Health and Human Services. https://wwwnc.cdc.gov/travel/destinations/list accessed on November 30, 2022.
National Travel Health Network and Centre. (n.d.). Country Information, UK Health Security Agency. https://travelhealthpro.org.uk/countries accessed on Sep 1, 2022.
Expert Committee for Travel Medicine. (2023). Health Advice for Travellers - Vaccinations. Swiss Society of Tropical and Travel Medicine. https://www.healthytravel.ch/vaccinations-3/ accessed on May 8, 2023.
Live vaccines
Australian Technical Advisory Group on Immunisation. (2022, May 19). Co-administration with other vaccines. In Australian Immunisation Handbook https://immunisationhandbook.health.gov.au/contents/vaccine-preventable-diseases/yellow-fever#coadministration-with-other-vaccines accessed December 17, 2022.
Nascimento Silva J.R., Camacho, L. A., Siqueira, M. M., et al. Mutual interference on the immune response to yellow fever vaccine and a combined vaccine against measles, mumps and rubella. Vaccine, 2011, 29(3). https://doi.org/10.1016/j.vaccine.2011.05.019
International Certificate of Vaccination or Prophylaxis
Centers for Disease Control and Prevention. (2022, August 3), Traveler’s Health, International Certificate of Vaccination or Prophylaxis (ICVP). U.S. Department of Health and Human Services https://wwwnc.cdc.gov/travel/page/icvp accessed on November 30, 2022.
Traveller’s Diarrhoea
General Information
Riddle, M.S., Connor, B. A., Beeching, N.J., DuPont, H.L., Hamer, D.H., Kozarsky, P., Libman, M., Steffen, R., Taylor, D., Tribble, D.R., Vila, J., Zanger, P and Ericsson, C.D. (2017). Guidelines for the prevention and treatment of travelers' diarrhea: a graded expert panel report. Journal of Travel Medicine, 24 (suppl_1):S57-S74. doi: 10.1093/jtm/tax026
LaRocque, R. and Harris, J.B. (2023). Traveler’s Diarhea: Treatment and Prevention. In T. W. Post, S. B. Calderwood and E. L. Baron (Eds.), UptoDate, available from https://www.uptodate.com/contents/travelers-diarrhea-clinical-manifestations-diagnosis-and-treatment?search=travelers%20diarrhea&topicRef=2709&source=see_link
Patient Handouts
Department of Health. (n.d.). Better Health Channel, Traveller’s Diarrhoea, State Government of Victoria, Australia. https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/travellers-diarrhoea accessed on November 30, 2022
Centers for Disease Control and Prevention. (2022, May 3). Traveler’s Health, Traveler’s Diarrhoea, U.S. Department of Health and Human Services https://wwwnc.cdc.gov/travel/page/travelers-diarrhea accessed on November 30, 2022
Polio
Outbreak and endemicity information
Global Polio Eradication Initiative. (n.d.). Outbreak Countries, https://polioeradication.org/where-we-work/polio-outbreak-countries/ accessed Jan 20, 2023
Department of Foreign Affairs and Trade. (n.d.). Smartraveller Destinations. Australian Government. https://www.smartraveller.gov.au/destinations accessed on April 5, 2023.
Ministry of Foreign Affairs and Trade. (n.d.). Safetravel – Travel Advisories by Destination. New Zealand Foreign Affairs and Trade. https://www.safetravel.govt.nz/travel-advisories-destination accessed on April 5, 2023.
Arthropod Borne Diseases
World Health Organisation. (2020, March 2). Vector Borne Diseases https://www.who.int/news-room/fact-sheets/detail/vector-borne-diseases accessed on November 1, 2022.
Webb, C. E. and Hess, I. M. R. (2016). A review of recommendations on the safe and effective use of topical mosquito repellents. Public Health Research and Practice. 2016;26(5). https://www.phrp.com.au/issues/december-2016-volume-26-issue-5/a-review-of-recommendations-on-the-safe-and-effective-use-of-topical-mosquito-repellents/ accessed on April 1, 2023.
Malaria
Centers for Disease Control and Prevention. (2022, September 13). Traveler’s Health, Disease Directory, Malaria. U.S. Department of Health and Human Services https://wwwnc.cdc.gov/travel/diseases/malaria accessed on April 6, 2023.
Fit for Travel. (n.d.). Malaria. Public Health Scotland https://fitfortravel.nhs.uk/advice/malaria#malaria accessed on September 1, 2022.
National Travel Health Network and Centre. (n.d.). Country Information, UK Health Security Agency. https://travelhealthpro.org.uk/countries accessed on Sep 1, 2022.
Prophylaxis
Gershman, M. D., Jentes, E. S., Stoney, R. J., Tan, K. R. and Arguin, P. M. (2021, December 13). Yellow Fever Vaccine and Malaria Prophylaxis Information, by Country. In G. W. Brunette and J. B. Nemhauser (Eds.), CDC Yellow Book 2020, Oxford University Press. https://wwwnc.cdc.gov/travel/yellowbook/2020/preparing-international-travelers/yellow-fever-vaccine-and-malaria-prophylaxis-information-by-country accessed April 6, 2023
Tan, K. R. and Arguin, P. M. (2019, July 1). Travel-Related Infectious Diseases: Malaria. In G. W. Brunette and J. B. Nemhauser (Eds.), CDC Yellow Book 2020, Oxford University Press. https://wwwnc.cdc.gov/travel/yellowbook/2020/travel-related-infectious-diseases/malaria accessed April 6, 2023.
Centers for Disease Control and Prevention. (2022, September 13). Traveler’s Health, Disease Directory, Malaria. U.S. Department of Health and Human Services https://wwwnc.cdc.gov/travel/diseases/malaria
Centers for Disease Control and Prevention. (2021, November 2). Malaria and Travelers, Malaria Information and Prophylaxis, by country. U.S. Department of Health and Human Services https://www.cdc.gov/malaria/travelers/country_table/a.html accessed on Sep 1, 2023.
Chiodini, P. L., Patel, D., Goodyer, L. and Ranson, H. (2023, February 8). Guidelines for malaria prevention in travellers from the United Kingdom, London: UK Health Security Agency. https://www.gov.uk/government/publications/malaria-prevention-guidelines-for-travellers-from-the-uk accessed on April 6, 2023.
Japanese Encephalitis
Australian Technical Advisory Group on Immunisation (ATAGI),(2022). Japanese Encephalitis. In Australian Immunisation Handbook https://immunisationhandbook.health.gov.au/contents/vaccine-preventable-diseases/japanese-encephalitis accessed April 1, 2023.
Dengue Fever
World Health Organisation. (2023). Dengue and severe dengue, https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue accessed March 3, 2023
Sharp, T. M., Perez-Padilla, J. and Waterman, S. H. (2019, July 1). Dengue. In G. W. Brunette and J. B. Nemhauser (Eds.), CDC Yellow Book 2020, Oxford University Press. https://wwwnc.cdc.gov/travel/yellowbook/2020/travel-related-infectious-diseases/dengue accessed November 1, 2023.
Centers for Disease Control and Prevention. (2020, July 14). Dengue, For Healthcare Providers. U.S. Department of Health and Human Services https://www.cdc.gov/dengue/healthcare-providers/index.html accessed November 1, 2023.
Chikungunya
World Health Organisation. (2022, December 8). Chikungunya https://www.who.int/news-room/fact-sheets/detail/chikungunya accessed December 1, 2022.
Centers for Disease Control and Prevention. (2023, January 26). Information for Health Care Providers. U.S. Department of Health and Human Services https://www.cdc.gov/chikungunya/hc/index.html accessed March 1, 2023.
Centers for Disease Control and Prevention. (2023, March 21). Areas at risk for Chikungunya. U.S. Department of Health and Human Services https://www.cdc.gov/chikungunya/geo/ accessed March 1, 2023.
Zika
World Health Organisation. (n.d.). Zika Virus Disease, https://www.who.int/health-topics/zika-virus-disease#tab=tab_1
Centers for Disease Control and Prevention. (2022, May 24). Zika Travel Information. U.S. Department of Health and Human Services https://wwwnc.cdc.gov/travel/page/zika-information accessed December 1, 2022.
Centers for Disease Control and Prevention. (2022, November 2). Zika Virus. U.S. Department of Health and Human Services https://www.cdc.gov/zika/ accessed December 1, 2022.
Centers for Disease Control and Prevention. (2018). For Healthcare Providers. U.S. Department of Health and Human Services https://www.cdc.gov/zika/hc-providers/index.html accessed December 1, 2022.
Yellow Fever
Maps
Centers for Disease Control and Prevention. (2019, June 24). Vaccination recommendations in Africa. In G. W. Brunette and J. B. Nemhauser (Eds.), CDC Yellow Book 2020, Oxford University Press. https://www.cdc.gov/travel-static/yellowbook/2020/map_4-13.pdf
Centers for Disease Control and Prevention. (2019, June 24). Vaccination recommendations in Americas. In G. W. Brunette and J. B. Nemhauser (Eds.), CDC Yellow Book 2020, Oxford University Press. https://www.cdc.gov/travel-static/yellowbook/2020/map_4-14.pdf
General Information
Gershman, M. D. and Staples, J. E. (2021), Yellow Fever. In G. W. Brunette and J. B. Nemhauser (Eds.), CDC Yellow Book 2020, Oxford University Press. https://wwwnc.cdc.gov/travel/yellowbook/2020/travel-related-infectious-diseases/yellow-fever accessed April 6, 2023.
World Health Organisation. (2019). Yellow Fever https://www.who.int/en/news-room/fact-sheets/detail/yellow-fever accessed April 6, 2023.
Pan American Health Organisation. (n.d.). Yellow Fever https://www.paho.org/en/topics/yellow-fever accessed April 6, 2023.
Australian Technical Advisory Group on Immunisation (ATAGI). (2022). Yellow Fever Requirements. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/contents/vaccination-for-special-risk-groups/vaccination-for-international-travellers#vaccines-required-by-the-international-health-regulations-or-for-entry-into-specific-countries accessed April 6, 2023.
Australian Technical Advisory Group on Immunisation (ATAGI). (2022). Yellow Fever. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/contents/vaccine-preventable-diseases/yellow-fever accessed April 6, 2023.
Department of Health and Aged Care, Commonwealth of Australia. (2023). Yellow Fever, https://www.health.gov.au/diseases/yellow-fever accessed April 6, 2023.
Department of Health, Australian Government. (2023). National Guidelines for Yellow Fever Vaccination Centres and Providers, https://www.health.gov.au/sites/default/files/2022-12/national-guidelines-for-yellow-fever-vaccination-centres-and-providers.pdf accessed April 6, 2023.
Te Whatu Ora Health New Zealand. (2023). Authorised Yellow Fever Vaccination Centres, https://www.tewhatuora.govt.nz/for-the-health-sector/health-sector-guidance/diseases-and-conditions/yellow-fever/authorised-yellow-fever-vaccination-centres/ accessed April 6, 2023.
Centers for Disease Control and Prevention. (2023, January 26). For Healthcare Providers. U.S. Department of Health and Human Services https://www.cdc.gov/yellowfever/healthcareproviders/index.html accessed April 6, 2023.
Public Health England. (2020). Yellow Fever: Guidance, Data and Analysis, https://www.gov.uk/guidance/yellow-fever-guidance-data-and-analysis accessed September 1, 2022.
Vaccine Recommendations
World Health Organisation. (2023). Country List, Country vaccination requirements and WHO recommendations for vaccination against yellow fever, poliomelitis, and malaria prophylaxis in international travellers.https://cdn.who.int/media/docs/default-source/travel-and-health/vaccination-requirements-and-who-recommendations-ith-2022-country-list.pdf accessed March 1, 2023.
Australian Technical Advisory Group on Immunisation (ATAGI). (2022). Yellow Fever. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/contents/vaccine-preventable-diseases/yellow-fever#travellers accessed on March 1, 2023.
Te Whatu Ora Health New Zealand. (2023). Yellow Fever, https://www.tewhatuora.govt.nz/for-the-health-sector/health-sector-guidance/diseases-and-conditions/yellow-fever accessed on March 1, 2023.
Training opportunities to become an accredited yellow fever vaccinator
Australian College of Rural and Remote Medicine https://mycollege.acrrm.org.au/search/find-online-learning/details?id=22729 accessed April 6, 2023.
The Immunisation Advisory Centre https://lms.immune.org.nz/user/login?destination=dashboard accessed April 6, 2023.
Rabies
Australian Technical Advisory Group on Immunisation. (2018). Rabies and other Lyssavirues. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/contents/vaccine-preventable-diseases/rabies-and-other-lyssaviruses accessed April 6, 2023.
World Health Organisation. (2023). Rabies. https://www.who.int/news-room/fact-sheets/detail/rabies accessed April 6, 2023.
World Health Organisation. (n.d.). Rabies. https://www.who.int/data/gho/data/themes/topics/rabies accessed April 6, 2023.
Furuya-Kanamori, L., Ramsey, L., Manson, M., Gilbert, B. and Lau, C. L. (2020). Intradermal rabies pre-exposure vaccination schedules in older travellers: comparison of immunogenicity post-primary course and post-booster. Journal of Travel Medicine. Nov 9;27(7) DOI: 10.1093/jtm/taaa006 accessed December 3, 2022.
Mills, D. J., Lau, C.L. and Weinstein, P. (2011). Animal bites and rabies exposure in Australian travellers. Medical Journal of Australia;195(11). https://www.mja.com.au/journal/2011/195/11/animal-bites-and-rabies-exposure-australian-travellers accessed December 3, 2022.
World Health Organisation. (2018). Rabies vaccines: WHO position paper – April 2018, Weekly epidemiological record, No 16,(93), 201–220. https://www.who.int/publications/i/item/who-wer9316 accessed April 6, 2023.
World Health Organisation. (n.d.). Evidence to Recommendation Table 4: time and dose sparing PrEP. https://cdn.who.int/media/docs/default-source/immunization/position_paper_documents/rabies/rabies-time-dose-sparing-prep.pdf?sfvrsn=fe81e0b4_2 accessed April 6, 2023.
Hepatitis B
Vaccine recommendations
Australian Technical Advisory Group on Immunisation. (2018). Travellers to hepatitis B endemic areas are recommended to receive hepatitis B vaccine in certain circumstance, in Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/recommendations/travellers-to-hepatitis-b-endemic-areas-are-recommended-to-receive-hepatitis-b-vaccine-in-certain-circumstances accessed on September 1, 2022.
Ministry of Health. (2022). Hepatitis B Vaccines, in Immunisation Handbook 2020. https://www.health.govt.nz/our-work/immunisation-handbook-2020/9-hepatitis-b#8-4 accessed on September 1, 2022.
Combined Hepatitis A & B vaccines
Australian Technical Advisory Group on Immunisation. (2021). Table. Combination hepatitis A-hepatitis B vaccines. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/resources/tables/table-combination-hepatitis-a-hepatitis-b-vaccines accessed on September 1, 2022.
Ministry of Health. (2021). Hepatitis A Vaccines, in Immunisation Handbook 2020. https://www.health.govt.nz/our-work/immunisation-handbook-2020/8-hepatitis#7-4 accessed on September 1, 2022.
HIV and Travel
The Global Database on HIV specific travel and residence restrictions. (n.d.). https://www.hivtravel.org accessed on September 1, 2022.
COVID-19
Travel Medicine Clinical Guidelines Australia and New Zealand. (n.d.). Australian COVID-19 International Travel Guidelines https://www.travelmedicineguidelinesanz.org/covid-19-information.php accessed on Nov 30, 2022.
Packing list for COVID-19
Travel Medicine Clinical Guidelines Australia and New Zealand. (n.d.). Packing List, https://www.travelmedicineguidelinesanz.org/covid-19-information.php#Packinglist accessed on Nov 30, 2022.
Meningococcal Disease
General Information
Mbaeyi, S. A. and McNamara, L. A. (2019, June 24). Meningococcal Disease. In G. W. Brunette and J. B. Nemhauser (Eds.), CDC Yellow Book 2020, Oxford University Press. https://wwwnc.cdc.gov/travel/yellowbook/2020/travel-related-infectious-diseases/meningococcal-disease accessed April 1, 2023.
Map
Mbaeyi, S. A. and McNamara, L. A. (2019, June 24). Map 4-10 Areas with frequent epidemics of meningococcal meningitis. In G. W. Brunette and J. B. Nemhauser (Eds.), CDC Yellow Book 2020, Oxford University Press. https://wwwnc.cdc.gov/travel/yellowbook/2020/travel-related-infectious-diseases/meningococcal-disease#map410 accessed April 1, 2023.
Vaccine recommendations
World Health Organisation. (n.d.). Meningococcal meningitis, https://www.who.int/teams/immunization-vaccines-and-biologicals/diseases/meningitis accessed April 6, 2023.
Australian Technical Advisory Group on Immunisation. (2022). Meningococcal Disease Traveller’s. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/contents/vaccine-preventable-diseases/meningococcal-disease#travellers accessed December 17, 2022.
Australian Technical Advisory Group on Immunisation. (2022). Requirement for traveller’s to Mecca. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/contents/vaccination-for-special-risk-groups/vaccination-for-international-travellers#requirements-for-travellers-to-mecca accessed December 17, 2022.
Australian Technical Advisory Group on Immunisation. (2021). Table. Recommendations for meningococcal vaccines for people at increased risk of meningococcal disease. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/resources/tables/table-recommendations-for-meningococcal-vaccines-for-people-at-increased-risk-of-meningococcal-disease accessed December 17, 2022.
Australian Technical Advisory Group on Immunisation. (2022). Meningococcal Disease. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/contents/vaccination-for-special-risk-groups/vaccination-for-international-travellers#meningococcal-disease accessed December 17, 2022.
Ministry of Health. (n.d.) Meningococcal Disease – Recommended immunisation schedule, in Immunisation Handbook 2020. https://www.health.govt.nz/our-work/immunisation-handbook-2020/13-meningococcal-disease#12-5 accessed on September 1, 2022.
Tuberculosis
High incident countries
New South Wales Health. (2023). List of Countries where tuberculosis (TB) is common, New South Wales Government. https://www.health.nsw.gov.au/Infectious/tuberculosis/Pages/high-incidence-countries.aspx accessed April 6, 2023.
World Health Organisation. (2022). Global Tuberculosis Report 2022. https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2022 accessed April 6, 2023.
Vaccine recommendations
Australian Technical Advisory Group on Immunisation. (2022). Tuberculosis – Travellers. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/contents/vaccine-preventable-diseases/tuberculosis#travellers accessed April 6, 2023.
Australian Technical Advisory Group on Immunisation. (2022). Tuberculosis – Other groups. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/contents/vaccine-preventable-diseases/tuberculosis#other-groups accessed April 6, 2023.
Australian Technical Advisory Group on Immunisation. (2022). Tuberculosis – Tuberculin skin testing before vaccination. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/contents/vaccine-preventable-diseases/tuberculosis#tuberculin-skin-testing-before-vaccination accessed April 15, 2023.
Australian Technical Advisory Group on Immunisation. (2022). Tuberculosis – Tuberculin skin testing before vaccination. In Australian Immunisation Handbook. https://immunisationhandbook.health.gov.au/recommendations/a-tuberculin-skin-test-tst-mantoux-before-bcg-vaccination-is-only-recommended-in-certain-circumstances-based-on-risk-factors-for-previous-tuberculosis-exposure accessed April 15, 2023.
Ministry of Health. (2022). Tuberculosis – Recommended Immunisation Schedule, in Immunisation Handbook 2020. https://www.health.govt.nz/our-work/immunisation-handbook-2020/21-tuberculosis#20-5 accessed April 6, 2023.
High Altitude Travel
Hackett, P. H. and Shlim, D. R. (2019, October 18). High-Altitude Travel and Altitude Illness. In G. W. Brunette and J. B. Nemhauser (Eds.), CDC Yellow Book 2020, Oxford University Press. https://wwwnc.cdc.gov/travel/yellowbook/2020/noninfectious-health-risks/high-altitude-travel-and-altitude-illness accessed April 6, 2023.
Altitude Physiology Expeditions. (n.d.). Altitude Sickness, https://www.altitude.org/altitude-sickness accessed April 6, 2023.
Luks, A. M. and Swenson, E.R. (2008). Medication and dosage considerations in the prophylaxis and treatment of high-altitude illness. Chest. 133(3):744e55
Luks, A. M., Auerbach, P. S., Freer, L., Grissom, C. K., Keyes, L. E., McIntosh, S. E., Rodway, G. W., Schoene, R. B., Zafren, K., & Hackett, P. H. (2019). Wilderness Medical Society Clinical Practice Guidelines for the Prevention and Treatment of Acute Altitude Illness: 2019 Update. Wilderness & environmental medicine, 30(4S), S3–S18. DOI: 10.1016/j.wem.2019.04.006
Altitude Illness. (2012). In Therapeutic Guidelines, Melbourne. Therapeutic Guidelines Limited. Available from https://www.tg.org.au accessed April 10, 2023.
Thromboemboli
Reyes, N.L., Beckman, M.G and Abe, K. (2019, June 24). Deep Vein Thrombosis and Pulmonary Embolism. In G. W. Brunette and J. B. Nemhauser (Eds.), CDC Yellow Book 2020, Oxford University Press. https://wwwnc.cdc.gov/travel/yellowbook/2020/travel-by-air-land-sea/deep-vein-thrombosis-and-pulmonary-embolism#box801 accessed April 6, 2023.
Centers for Disease Control and Prevention. (2022, June 9). Venous thromboembolism – Blood Clots and Travel: What you need to know. U.S. Department of Health and Human Services https://www.cdc.gov/ncbddd/dvt/travel.html accessed April 6, 2023.
Education for practitioners
Training opportunities to become an accredited yellow fever vaccinator
Australian College of Rural and Remote Medicine https://mycollege.acrrm.org.au/search/find-online-learning/details?id=22729 accessed April 6, 2023.
The Immunisation Advisory Centre https://lms.immune.org.nz/user/login?destination=dashboard accessed April 6, 2023.
Travel Medicine training
James Cook University. (n.d.). Graduate Certificate of Tropical Medicine, https://www.jcu.edu.au/courses/graduate-certificate-of-travel-medicine accessed April 6, 2023.
University of Otago. (n.d.). Postgraduate Certificate in Travel Medicine, https://www.otago.ac.nz/courses/qualifications/pgcerttravmed.html accessed April 6, 2023.
Royal College of Physicians and Surgeons of Glasgow. (n.d.). Professional Development Certificate in Travel Medicine. https://rcpsg.ac.uk/travel-medicine/qualifications-in-travel-medicine/professional-development-certificate-in-travel-medicine accessed April 6, 2023.
Royal College of Physicians and Surgeons of Glasgow. (n.d.) Travel Medicine, https://rcpsg.ac.uk/travel-medicine/qualifications-in-travel-medicine accessed April 6, 2023.
Online and other useful resources
Department of Health and Aged Care. (2023). National Immunisation Programme Schedule, Australian Government. https://www.health.gov.au/topics/immunisation/when-to-get-vaccinated/national-immunisation-program-schedule?language=und accessed April 6, 2023.
Ministry of Health. (2020). Immunisation Handbook 2020. Wellington: Ministry of Health. https://www.health.govt.nz/our-work/immunisation-handbook-2020 accessed April 6, 2023.
World Health Organisation. (n.d.) https://www.who.int
International Society of Travel Medicine. (n.d.) https://www.istm.org/index.asp
Asia Pacific Travel Health Society. (n.d.) https://www.apths.org accessed April 6, 2023.
Epiwatch (n.d.) https://www.epiwatch.org accessed April 6, 2023.
Healthmap (n.d.) https://healthmap.org/en/ accessed April 6, 2023.
National Travel Health Network and Centre. (n.d.). Country Information, UK Health Security Agency. https://travelhealthpro.org.uk/countries accessed on Sep 1, 2022.
Prepared by Frances Daily, published 14 August 2023