Download the Japanese Encephalitis Guidelines
Please click here to download the Japanese Encephalitis Guidelines.
Purpose of Guidelines
The purpose of this guideline is to aid travel health practitioners to consider the risk of an individual traveller to Japanese Encephalitis (JE) and consider if vaccination should be considered along with other measures for prevention.
Pre-travel Health Risk Assessment
Travellers from Australia and New Zealand are recommended to have a routine pre-travel consultation, including information on JE, where required. Each traveller should consult with a health practitioner experienced in travel medicine and more than one consultation may be required due to the complexity of travel with the evolution of disease outbreaks. When considering the risk of JE to a traveller we need to consider:
- Are they travelling to a region with risk of JE?
- What is the risk to an individual of acquiring JE if they are travelling to an endemic area?
- Is the traveller likely to undertake activities which may increase the risk of JE?
- Is there sufficient risk to consider vaccination and what do we need to inform the traveller about the vaccine prior to this decision being made?
- What other personal mitigation and preventive measures are available to reduce risk?
- Advice on illness overseas or on return to Australia and New Zealand.
1. Endemic areas for JE
JE is a viral disease, caused by an RNA flavivirus, spread through mosquito bites and is more common in areas of increased mosquito activity. It is endemic to Asia and the Torres Strait but has been more recently confirmed in the eastern states of Australia. The risk of JE in Aotearoa New Zealand is low.
Figure 1. Endemic areas for JE

Figure 1. Japanese encephalitis virus is endemic throughout tropical and temperate areas of Asia, up to the 45th parallel. In Australia, local transmission prior to 2021 has been confined to the outer islands of the Torres Strait and Cape York, where it was identified in 1995. As of May 2022, distribution may have expanded to include large parts of Queensland, New South Wales, Victoria and South Australia. This figure was adapted from the WHO under a creative commons licence and is taken, with permissions, from the QIMR Berghofer website.
2. Risk of infection
JE is spread among humans by the bite of a Culex species of mosquito, see life cycle Figure 2, after they are infected by feeding on viraemic animal vectors kept in areas near rice paddies and piggeries. The mosquito habitats are rural and semi-rural areas of tropical and temperate regions, and their breeding grounds are stagnant waters. Peak biting is usually between dusk and dawn. The main mosquito vector for JE in Asia and Australia is Culex tritaeniorhynchus.
Figure 2. Life cycle of the JE virus
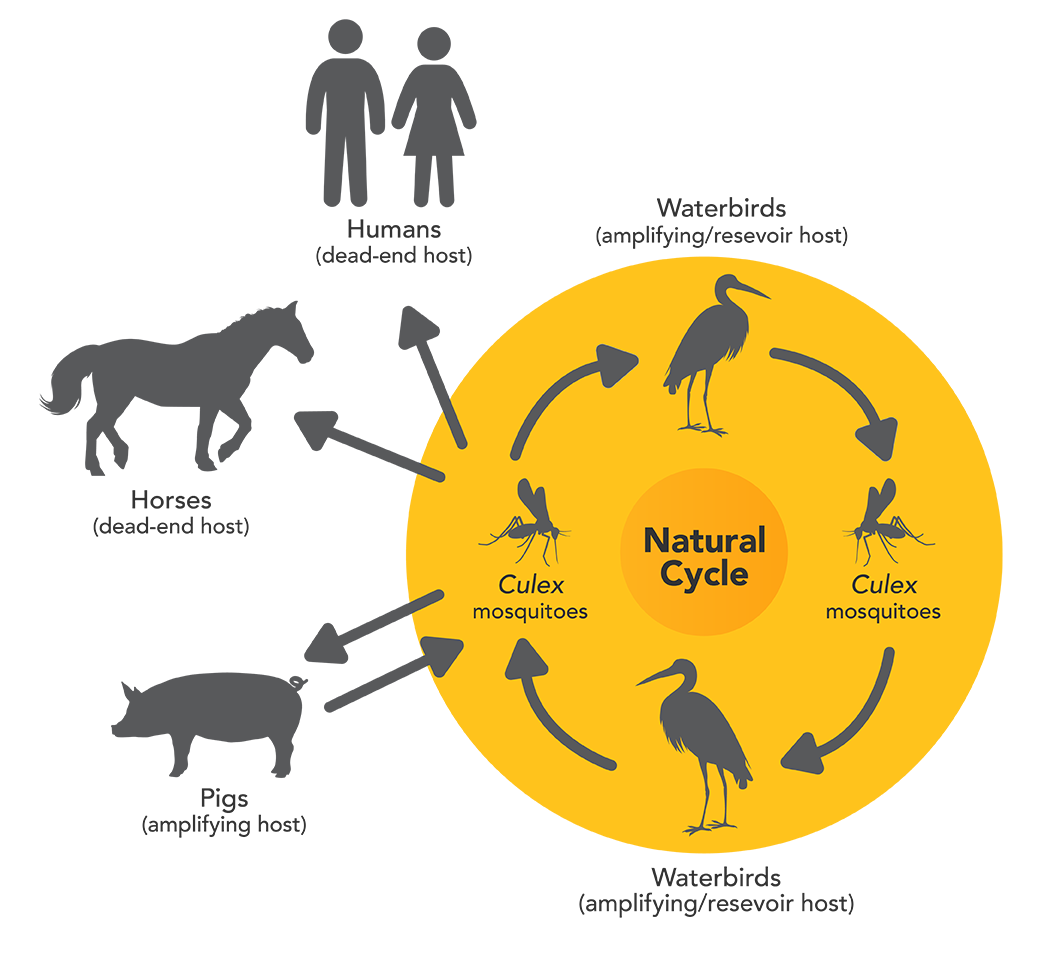
Image source: Department of Agriculture, Water and the Environment (DAWE)
Animals can be infected with the JE virus (JEV) from a bite from an infected mosquito vector, but they cannot transmit the virus to humans directly.
- An amplifying host is one in which infectious agents multiply rapidly to high levels, providing an important source of infection for vectors, in this case, mosquitoes. JE infection is amplified in cycles between infected mosquito vectors, the main reservoirs (waterbirds) and the amplifying hosts (mostly pigs). Pigs do not show signs of JEV infection, but the virus can cause abortion and stillbirth of their offspring.
- A dead-end host is one from which infectious agents are not transmitted to other susceptible hosts. Humans and other large animals such as horses do not develop sufficient levels of JE viraemia to infect mosquito vectors and transmit onward to other potential hosts. JE cannot be transmitted between humans, or by eating meat or other products from an infected animal.
The risk of JE to travellers is low, but infection can be devastating. While for most humans the infection is most often asymptomatic, it can result in severe disease and death. Figure 3 demonstrates the risk of disease in a traveller estimated to be 1 in 1 million per month of travel. Although symptomatic JE is rare, the case-fatality rate among those who develop encephalitis can be as high as 30% and permanent neurologic or psychiatric sequelae can occur in 30% to 50% of survivors. The annual incidence of clinical disease varies both across and within endemic countries, ranging from <1 to >10 per 100 000 population or higher during outbreaks.
Figure 3. Vaccine preventable disease travel health risks: Estimated incidence per month in lower income countries.
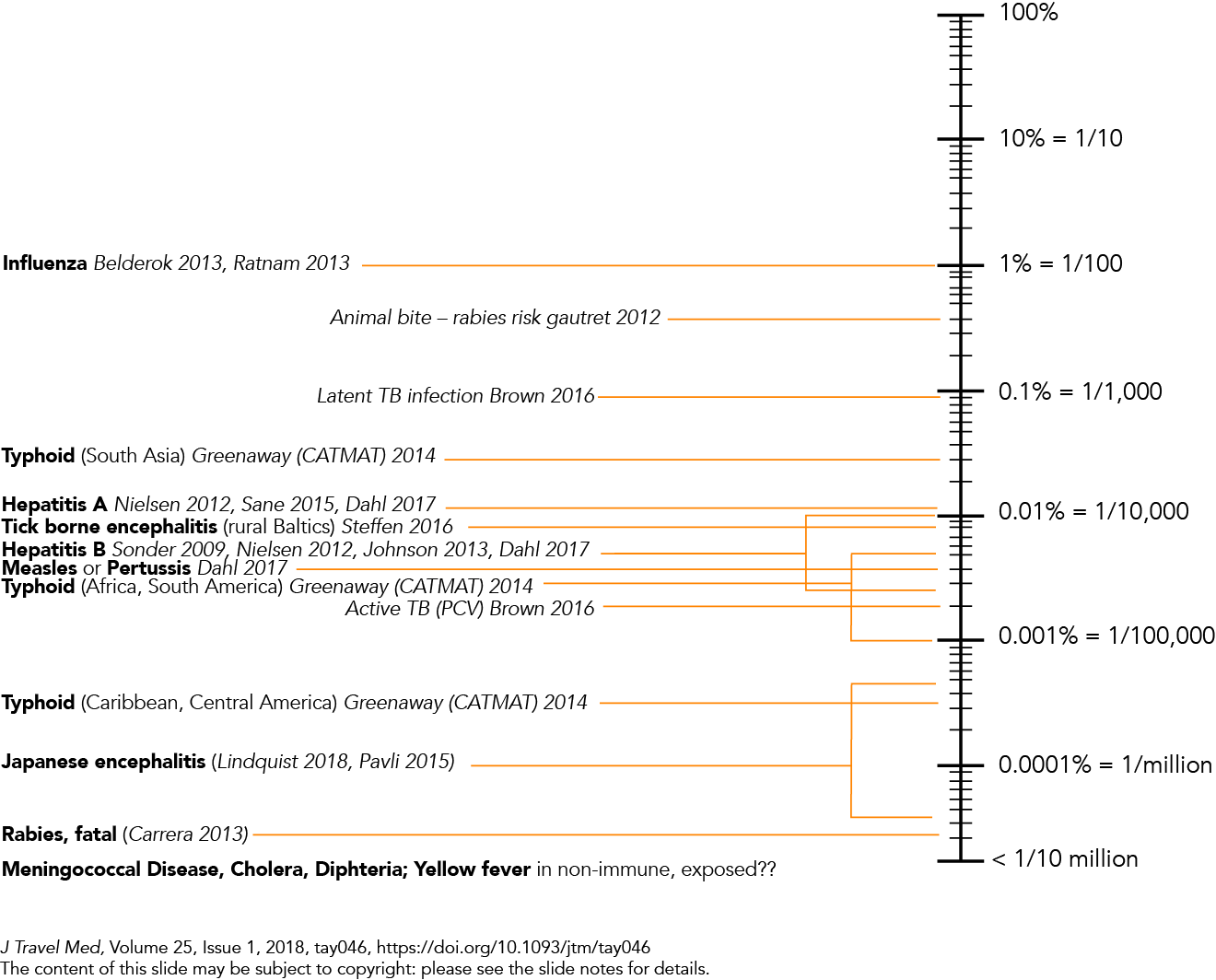
J Travel Med, Volume 25, Issue 1, 2018, tay046, https://doi.org/10.1093/jtm/tay046
3. Activities that increase risk
Considerations for risk for the individual traveller in the pre-travel consultation:
- Length of travel
- Cumulative risk over time (multiple trips)
- Season of travel – wet or dry
- Accommodation type – air-conditioned hotel or camping for example.
- City vs peri-urban vs rural
- Time likely to be spent outside from dusk to dawn – shift workers or travellers who may be camping and sitting around a campfire at night.
Risk of contracting JE is cumulative, and consideration should be given to lifetime risk, not just the trip at hand i.e., people who visit locations multiple times for short periods.
Individuals working in endemic areas need to be assessed for risk and it may be considered part of the employers duty of care to their employee if they are to work in risk areas.
Table 1. Risk Factors for JE
| Who is at greater risk of exposure to JE | Travellers spending one month or more in endemic areas in Asia, PNG and Torres Straits during wet season. |
| Other Factors |
Asian temperate or subtropical regions: epidemics occur during the summer or wet season (April-May & September - October). Tropical regions: disease occurs throughout the year, more prominent during in wet season. |
| Activities that increase chances of JE infection |
|
All of these factors should be considered when determining risk.
Click here for a JE risk calculator based on best available published research www.vaxical.com
4. Vaccination Considerations
Two vaccines for JE are available in Australia; Imojev® a live attenuated vaccine, and Jespect® an inactivated JE vaccine. In New Zealand, Imojev has recently been licenced for use. JEspect is also available.
Each vaccine has different:
- Registered age groups
- Vaccine schedules
- Booster dose requirements
- Contraindications for use
In general within Australia, Imojev is the preferred option in adults (>18yrs) as a single dose and once given it is considered to give lifelong cover. Imojev is registered for use in babies 9 months and older. In under 18’s a booster is needed after 18 months to 2 years. As a live attenuated vaccine, the appropriate check list applies i.e. must be given on the same day or 28 days apart from other live vaccines (such as MMR, Varivax, BCG, yellow fever vaccine).
JEspect is the preferred vaccine in individuals in which Imojev is contraindicated. It is a 2 dose regime given, one month apart (a rapid schedule can be given if required). In adults (>18yrs), a booster is given after 2 years if at continuing risk. This vaccine can also be used in infants from 2 months of age in a reduced dosage. More details are in the Australian Immunisations Handbook.
Clinicians should discuss these considerations with travellers and should refer to the Australian Immunisation Handbook which contains extensive discussion on the different vaccines https://immunisationhandbook.health.gov.au/contents/vaccine-preventable-diseases/japanese-encephalitis#vaccine-information for further detail to determine which vaccine is preferable. There are no current immunisation guidelines for Imojev in New Zealand.
The cost of the vaccine needs to be considered also as it is not insignificant and may be a deciding factor for some travellers.
Traditionally JE vaccine has been recommended for travellers to endemic areas for a month or more in the transmission season. It was rarely offered for anyone on one off short package holidays to the resorts and capital cities in Asia. However, due to cases occurring in short term travellers, the Australian Immunisation Handbook now includes discussion with all travellers visiting JE endemic areas.
JE vaccination is not routinely recommended for travellers spending less than one month in endemic areas. However, there are confirmed cases in travellers who have acquired JE in a shorter timeframe.
Vaccination should be considered for shorter-term travellers, particularly if:
- the travel is during the wet season
- there may be ongoing travel to at-risk areas
- there is considerable outdoor activity during the travel
- the traveller is staying in accommodation without air-conditioning, insect screens or bed nets.
Research has and is being undertaken in Australia to establish effectiveness of intradermal vaccination as a dose sparing measure in the event of an outbreak. This route is not recommended to be used by GPs as it is only for use by public health officials in outbreak settings. ATAGI has released information for intradermal use if required in this setting: https://www.health.gov.au/sites/default/files/2022-12/atagi-statement-on-the-intradermal-use-of-imojev-japanese-encephalitis-vaccine.pdf. Information on the immunogenicity of a single fractional intradermal dose of Japanese encephalitis live attenuated chimeric vaccine is available at: https://europepmc.org/article/med/36308439.
5. Personal Prevention
There are 2 ways to prevent JE:
- Receive vaccination for JE
- Avoid being bitten by mosquitoes.
It is essential travellers are aware of the personal protective measures used to reduce the risk of insect borne diseases in general. It is particularly important for those at risk of exposure to JE who choose not to be vaccinated. JE is not the only vector borne disease prevalent in most JE endemic areas.
In general, travellers should be encouraged to wear clothing that covers as much of the body as possible and, in lighter colours. Apply repellent to all exposed areas evenly, as directed by the product. Various insect repellent formulations are available:
- DEET (Diethyltolumide)
- Picaridin
- OLE (oil of lemon eucalyptus)
They are available in different concentrations of the active ingredient. All are effective, the strength influences how frequently they must be applied.
Personal Protective measures for mosquitoes are outlined here:
https://www.health.nsw.gov.au/Infectious/factsheets/Pages/mosquito.aspx
Further in depth detail on Personal Protective measures for mosquitoes are in the Arthropod Borne Disease Guideline.
It is important that all travellers are educated on modes of transmission and how to prevent JE.
Returning to Australia or New Zealand
It is also important practitioners reinforce to travellers the need to seek medical attention if they develop a fever or becomes unwell during or after travel. This will ensure early and correct diagnosis of febrile illnesses in travellers.
In those that develop symptoms, the time from infection with JEV until illness onset is typically 5-15 days:
- Fever, headache, and vomiting.
- Mental status changes, neurologic symptoms, weakness, and movement disorders might develop over the next few days.
- Seizures are common, especially among children.
- Among patients who develop encephalitis, 20%–30% die.
- Although some symptoms improve after the acute illness, 30%–50% of survivors continue to have neurologic, cognitive, or psychiatric symptoms.
Treatment of JE is supportive only and beyond the scope of this document.
Public health management
In Australia JE is a notifiable disease and was temporarily made a Communicable Disease Incident of National Significance after the outbreak began in Australia in 2020.
On 16th June 2023 it was declared that JEV is no longer a Communicable Disease Incident of National Significance (CDINS). Australia’s coordinated response to the outbreak is being wound back, with states and territories well placed to continue to manage any ongoing risk - https://www.health.gov.au/news/statement-on-the-end-of-japanese-encephalitis-virus-emergency-response?language=en. Further information on JE can be found at: https://www.health.gov.au/diseases/japanese-encephalitis.
State and territory public health authorities can provide advice on the public health management of JE, including management of cases.
- QLD - https://www.health.qld.gov.au/system-governance/contact-us/contact/public-health-units
- NSW - https://www.health.nsw.gov.au/Infectious/Pages/phus.aspx
- ACT - https://www.health.act.gov.au/contact-us
- VIC - https://www.health.vic.gov.au/local-public-health-units
- TAS - https://www.health.tas.gov.au/contact-us
- SA - https://www.sahealth.sa.gov.au/wps/wcm/connect/public+content/sa+health+internet/public+health/public+health
- NT - https://health.nt.gov.au/professionals/centre-for-disease-control/cdc-contacts
- WA - https://ww2.health.wa.gov.au/Articles/A_E/Contact-details-for-regional-population-public-health-units
In New Zealand whilst the disease is not currently notifiable, it will need to be notified. Medical practitioners should immediately notify the Ministry of Health Communicable Diseases Team.
https://www.legislation.govt.nz/act/public/1956/0065/latest/DLM308729.html?search=ts_act_health+act_resel&p=1#DLM308729
Community and Public Health - https://www.cph.co.nz/your-health/infectious-diseases/
Local health websites - https://www.tewhatuora.govt.nz/keeping-well/health-info-for-public/district-health-websites/
Resources
- More than devastating—patient experiences and neurological sequelae of JE. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6792067/
- Recent cases of JE have been reported in Australia:
https://www.health.gov.au/health-alerts/japanese-encephalitis-virus-jev/about
https://www.health.gov.au/resources/collections/nndss-public-datasets - https://www.health.gov.au/sites/default/files/2023-06/joint-national-japanese-encephalitis-virus-outbreak-response-plan.pdf
- NCIRS Japanese Encephalitis - A learning resource for registered nurses and midwives
https://www.ncirs.org.au/sites/default/files/2022-11/NCIRS%20Japanese%20encephalitis%20learning%20resource_v2_18_11_22.pdf - Low uptake of Japanese encephalitis vaccination among Australian travellers. https://academic.oup.com/jtm/article/28/3/taaa232/6031799
- Comparison of immunogenicity and safety of licensed Japanese encephalitis vaccines https://espace.library.uq.edu.au/view/UQ:0bcd6c9
References
- Furuya-Kanamori L, Gyawali N, Mills DJ, Hugo LE, Devine GJ, Lau CL. The Emergence of Japanese Encephalitis in Australia and the Implications for a Vaccination Strategy. TropicalMed. 2022;7(6):85.
- Mills DJ, Lau CL, Furuya-Kanamori L. Low uptake of Japanese encephalitis vaccination among Australian travellers. Journal of Travel Medicine. 2020;taaa232.
- Australian Government. Department of Health and Aged Care. Japanese encephalitis virus (JEV) vaccines. Available at: https://www.health.gov.au/health-alerts/japanese-encephalitis-virus-jev/vaccines
- New South Wales Government. Japanese encephalitis fact sheet. Available at: https://www.health.nsw.gov.au/Infectious/factsheets/Pages/japanese_encephalitis.aspx
- Centers for Disease Control and Prevention. Yellow Book: Japanese Encephalitis. Available at: https://wwwnc.cdc.gov/travel/yellowbook/2020/travel-related-infectious-diseases/japanese-encephalitis
- World Health Organization. Japanese encephalitis (Factsheet). Available at: https://www.who.int/news-room/fact-sheets/detail/japanese-encephalitis
Prepared by Edith Torricke, published 14 August 2023